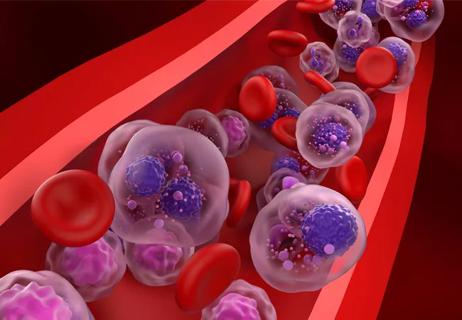
Study of 401,576 patients reveals differences in cancer burdens as well as overall survival

There are distinct differences in adverse events patients around the world experience during multiple myeloma treatment, according to data presented at the 2023 American Society of Clinical Oncology (ASCO) annual meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By mining records from 401,576 patients across 129 countries and 27 phenotypic systems in the FDA Adverse Event Reporting System, researchers identified differences in cancer burden and toxicities experienced by different racial and ethnic populations as well as other patient groups, such as those living in rural areas.
This first-of-its-kind global perspective on the real-world experiences of patients with multiple myeloma revealed that drug toxicities are affected by a wide array of factors, including geographic location (i.e., proximity to a major academic center), sex, genetics, comorbidities, financial literacy, genetics and epigenetic modification as well as dosing and regimen. Additionally, patients in various countries have access to different treatments, and those medications may be administered differently in that region.
“Delving into the causes of these differences will hopefully help to improve health outcomes for all,” says Shahzad Raza, MD, lead author and a myeloma specialist at Cleveland Clinic Cancer Institute.
For example, financial toxicity is another major factor affecting patient experiences, which may vary considerably depending on what medications a patient’s insurance covers and the out-of-pocket expenses they have. “Many patients don’t take treatment because they think it’s going to be a lot of money for them, which is often not true because there are a lot of resources available to address the situation,” says Dr. Raza.
The researchers found that:
Advertisement
In some cases, there are clues about why these toxicity clusters exist, as is the case with cardiovascular toxicities, which may be due in part to lifestyle and dietary issues in North America. Likewise, patients in Europe may be more prone to peripheral neuropathy due to the prevalence of older medications like thalidomide, which is known for this side effect. In other instances, it’s unclear why these toxicities are more frequent in certain regions, and more research is needed to determine whether this is due to genetics or other factors.
“When you put this data into perspective globally and see that there are huge differences based on a patient’s country of origin, the country’s access to treatments and more, it’s apparent there are many pieces of the equation that need to be resolved,” says Dr. Raza. “Each needs to be evaluated individually. Otherwise we’ll never have a good idea of how to optimize treatment for all patients.”
Knowing that the use of lenalidomide and melphalan in autologous stem cell transplants can increase the risk of secondary cancers in the long run, the biostatisticians and computational mathematicians involved in the study examined the rates of occurrence across regions.
Advertisement
Although the study didn’t factor in toxicities related to advanced treatments like CAR T-cell and bispecific therapies, it’s clear that their limited availability is likely to exacerbate differences. CAR T-cell therapy is only available at large academic centers due to the complexity of managing side effects. Similarly, bispecific therapy is administered only in hospitals. Doctors in community settings aren’t trained in these highly engineered treatments, so patients who live far from academic centers face additional hurdles accessing these treatments.
The lack of heterogeneity in multiple myeloma clinical trials leads to many unknowns about treating different populations. “Clinical trials across the globe lack these answers and for now we need to rely on registry data and retrospective data and interpreting the data based on the cross-trial comparisons,” says Dr. Raza. “Clinical trials show that multiple myeloma drugs can have a 90% response rate, but the majority of trial participants are Caucasian. Since we don’t have a wider variety of populations included in trials, we’re left to interpret these results and whether this is going to work the same way for other communities.”
Fortunately, more people are becoming aware of this issue and the importance of achieving better trial representation, says Dr. Raza. “That’s leading to more funding and social support. I think that’s going to change outcomes in the long run.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Phase 2 study brings pivotal advances in treatment efficacy and safety for the most challenging-to-treat population

Making sense of the fast-moving treatment landscape

Explaining common misconceptions about chimeric antigen receptor therapy

Clinicians share practices to streamline initiation of care

Prediction and bioinformatic data could prove valuable for therapeutic interventions targeting this malignancy

Findings from large database important to inform clinical practice
Despite sicker patients, response rates of teclistamab in a real-world study were similar to those from a pivotal clinical trial