Bcl-xL inhibitors may help overcome this complication
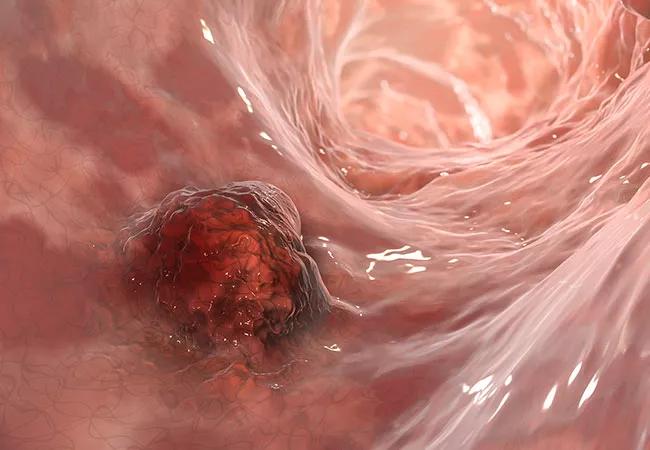
DNA-damaging therapies for colorectal cancer (CRC) can confer resistance to chemotherapy by promoting nuclear translocation of the protein myeloid cell leukemia (MCL1). Evidence suggests that this chemoresistance may be overcome by co-treating the disease with Bcl-xL inhibitors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recent studies in murine models of inflammatory CRC and patient-derived xenografts reveal that chemotherapy drives MCL1 from its canonical mitochondrial localization to the nucleus to cause chemoresistance, explains Brian Gastman, MD, study investigator and Surgical Director of the Melanoma and High-Risk Skin Cancer Program at Cleveland Clinic Cancer Center. The findings were published in Cell Death and Disease.
MCL1 is an anti-apoptotic member of the Bcl2-2 family that is essential for the survival of several cell lineages, including malignant cells. Previous research demonstrating that MCL1 could induce chemoresistance in CRC focused on the role of MCL1 in tumor mitochondria.
“MCL1 has not one but two components that can promote cancer growth and reduce the efficacy of chemotherapy,” says Dr. Gastman. “A new understudied feature of MCL1 works outside the mitochondria, traveling toward the nucleus.” Through immunostaining, both doxorubicin and oxaliplatin were found to stimulate trafficking of MCL1 from mitochondria to the nucleus in CRC cell lines.
Researchers also discovered new binding partners to MCL that allow it to move from the mitochondria to the nucleus. For the first time, their findings show that MCL1 accumulates in the nucleus in response to chemotherapy through a pathway that is dependent on an interaction between the proteins alpha-enolase and calmodulin. This is the first disclosure of the mechanism by which MCL1 moves from its classical mitochondrial compartment.
Advertisement
Another discovery was that MCL1 nuclear translocation was sensitive to the inhibition of calmodulin. Treatment of MCL1 cells with calmodulin inhibitors followed by treatment with doxorubicin showed that calmodulin activity was required for doxorubicin-induced MCL1 nuclear translocation and chemoresistance.
From immunohistochemical examination of CRC tumor biopsies from patients, the investigators also established a cooperative role between MCL1 and Bcl-xL, a transmembrane anti-apoptotic protein in the mitochondria, in the maintenance and progression of human CRC. Mitochondrial and intra-nuclear staining revealed the co-expression of MCL1 and Bcl-xL; high levels of this co-expression were more common in late stages of CRC compared with early stages.
This latter discovery has therapeutic potential by exploiting synthetic lethality between DNA-damaging agents and commercially available Bcl-xL-selective inhibitors. “Targeting CRC with Bcl-xL inhibitors does not work very well,” says Dr. Gastman. “But once you move MCL-1 out of the mitochondria, Bcl-xL inhibitors work. This is an exciting finding! There are chemotherapies that encourage MCL-1 to leave the mitochondria; so, in theory, we showed that off-the-shelf chemotherapies and Bcl-xL inhibitors could be used to kill CRC.”
Targeting the pathways responsible for MCL1 translocation from the mitochondria to the nucleus is another potential therapeutic strategy. “If we can block MCL1 along the path, we could have our cake and eat it too, meaning that we don’t want MCL1 to work in the mitochondria and we don’t want MCL1 to work in the nucleus,” he explains. “From a therapeutic design, we may not be able to stop MCL1 from moving to the nucleus, but we may be able to block it there. This is why it’s so important to understand what MCL1 is doing in the nucleus.” Identification of the binding proteins alpha-enolase and calmodulin are helping in this regard.
Advertisement
Targeting MCL in the mitochondria had been abandoned because it induced major cardiac toxicity, but blocking the pathway involved in MCL1 translocation from the mitochondria to the nucleus could lead to the re-emergence of MCL1-targeting agents, he says.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors