Study highlights the value of quantitative ultra-widefield angiography
The number of people with diabetes mellitus is estimated to reach 700 million worldwide by 2045, more than double the current number. Diabetic retinopathy (DR) is one of the most common complications of diabetes. It also is one of the main causes of preventable vision loss.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Although anti-VEGF therapy can help reduce DR severity, it remains a challenge to identify patients who would benefit from treatment when they do not have diabetic macular edema or proliferative disease,” says Justis P. Ehlers, MD, Director of the Tony and Leona Campane Center for Excellence in Image-Guided Surgery and Advanced Imaging Research at Cleveland Clinic Cole Eye Institute.
While the diabetic retinopathy severity scale (DRSS) is well-established and considered the gold standard, new imaging technologies and feature assessment tools may provide an opportunity for more precise severity scales that inform clinicians on treatment need or likelihood of response, he notes.
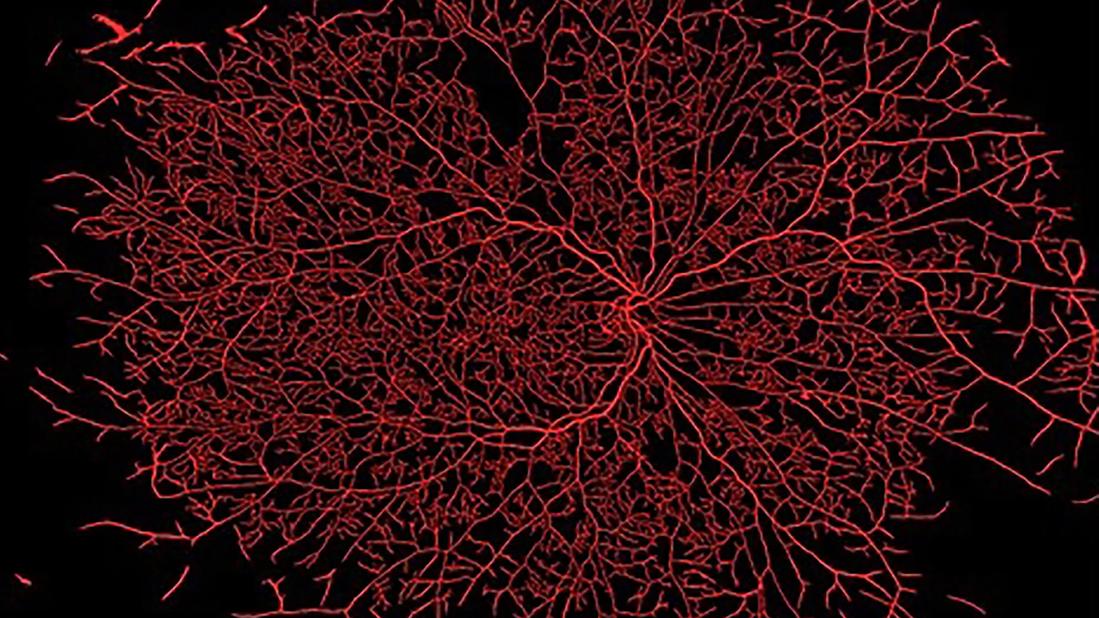
For the past few years, Dr. Ehlers and his research team have been working on innovative ways to characterize retinal disease based on imaging features, particularly the ability to better quantify and describe the changes in retinal vascular disease such as DR and diabetic macular edema. Quantitative ultra-widefield fluorescein angiography (qUWFA) has been a specific area of interest.
To evaluate how more enhanced assessment of qUWFA could aid understanding of DR and its response to anti-VEGF therapy, the team performed a post hoc analysis of patients in the PRIME trial. The PRIME trial was a prospective randomized trial comparing real-time treatment of DR based on DRSS compared to quantitative leakage index. The post hoc analysis focused on a wider spectrum of qUWFA features in these patients with DR but without diabetic macular edema. The results of this analysis were published in Ophthalmology Retina.
Advertisement
Over one year, a machine-learning image-analysis platform assessed the trends of qUWFA biomarkers and therapeutic response to aflibercept in 40 eyes from 40 patients with Type 1 or Type 2 diabetes, a DRSS level of 47A to 71A, and best-corrected visual acuity of 20/800 or better.
The analysis included panretinal leakage index measurement, microaneurysm count, ischemic index, and differentiation between generalized and perivascular leakage phenotypes in panretinal and macular regions.
“What we’ve seen in previous studies is that quantitative leakage may be one of the most important biomarkers for predicting risk of progression in diabetic retinopathy and risk of vision-threatening complications,” says Dr. Ehlers. “This suggests that the amount of leakage present may be the leading indicator of overall disease activity.”
The analysis also examined the associations of these qUWFA metrics with time to two-step DRSS improvement and number of treatment-free days by randomizing patients into two treatment arms. Patients in the DRSS-guided arm were treated based on their clinical appearance while those in the panretinal leakage index-guided arm were treated based on their quantitative angiography.
The study found that ongoing treatment with aflibercept, whether given as needed based on clinical appearance or quantitative angiography criteria, resulted in a substantial decrease in quantitative leakage.
Patients with more perivascular leakage were able to go longer between aflibercept injections, and those with lower generalized leakage had quicker responses to treatment.
Advertisement
“As we were able to characterize the types of leakage, whether perivascular or generalized, we saw different patterns in patient response,” says Dr. Ehlers. “This suggests that the vascular leakage phenotype may have important implications for the underlying mechanism and potential response to anti-VEGF therapy.”
The team also reported a significant reduction in microaneurysm counts in both patient groups over the one year of aflibercept therapy. Additionally, although not clearly clinically significant, ischemia appeared to be slightly improved to stable overall.
Studies have shown that angiography provides a more extensive assessment of blood vessel pathology that may be affected by DR and, thus, should play a role in DR management, says Dr. Ehlers.
“We’ve become a very OCT-driven subspecialty, and while I absolutely think OCT has a critical role, in retinal vascular diseases like diabetic retinopathy, it’s not uncommon to find significant discordance between what’s seen clinically and what is being identified angiographically,” he says.
At a minimum, Dr. Ehlers says angiographic features can help clinicians decide if they need to see a patient sooner. In his own practice, he uses ultra-widefield fluorescein angiography in patients with at least moderate DR “because it gives us so much more data on their amount of disease burden.”
One of the unique aspects of the study, a collaboration with Retina Consultants of Texas, was that patients received monthly ultra-widefield angiograms rather than conventional six-month or yearly imaging. The images were immediately transmitted to the central reading center at the Cole Eye Institute, where they were analyzed for quantitative parameters.
Advertisement
“Within one hour, we were able to tell the retina specialists in Texas whether or not each patient needed treatment,” says Dr. Ehlers. “This demonstrated real-time use of this type of technology.”
Dr. Ehlers believes the recent analysis supports the need to improve DR management.
“Anti-VEGF therapy is an amazing treatment to improve the overall appearance of diabetic retinopathy, but many of these patients may not need to be treated as they might be at low-risk for progression while others may be going undertreated,” he says. “Clinicians need better tools to identify which patients are at greatest risk so that we can approach treatment decisions with a higher degree of precision.”
Advertisement
Advertisement

Association revises criteria for the diagnosis and resolution of severe conditions

What to consider in the management of euglycemic DKA

Less than 50% of patients with diabetes get appropriate ophthalmic screening through primary care referrals

Familiarity will enhance its accessibility for patients with diabetes

New study counters earlier findings linking drugs with eye disease

Longevity in healthcare, personal experiences may provide caregivers with false sense of confidence

Maternal-fetal medicine specialists, endocrinologists and educators team up

Spinal cord stimulation can help those who are optimized for success