Study shows MRI infarct growth surges thereafter
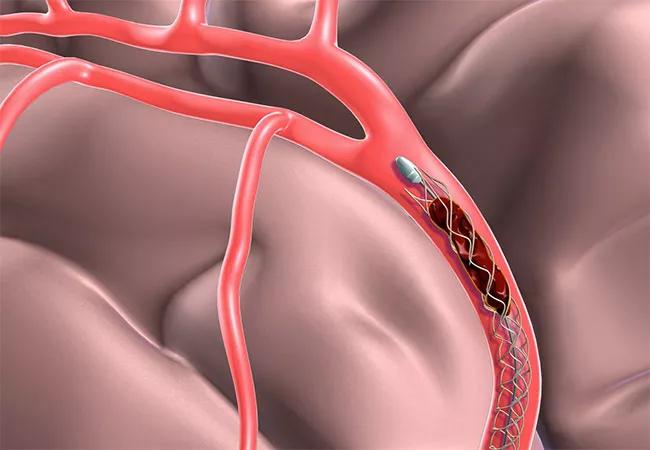
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0dbb9726-d88d-4a6f-9726-64b45e3ec4d2/20-NEU-062-mechanical-thrombectomy-for-stroke-650x450-1_jpg)
20-NEU-062 mechanical-thrombectomy-for-stroke 650×450
In patients undergoing mechanical thrombectomy for emergent large vessel occlusion (ELVO), infarct growth on MRI is significantly associated with both longer procedural time and increasing number of procedural passes attempted, according to a retrospective Cleveland Clinic study presented at the 2020 International Stroke Conference (ISC 2020) this week.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It has been recognized that longer procedure times generally result in more brain damage and worse clinical outcomes in patients with ELVO, but the direct effect on infarct growth has been uncertain, as has the specific contribution of the number of passes attempted to achieve recanalization,” says the study’s senior author, M. Shazam Hussain, MD, Director of Cleveland Clinic’s Cerebrovascular Center.
To shed light on these questions, he and colleagues reviewed consecutive patients presenting with ELVO to Cleveland Clinic’s comprehensive stroke center from January 2016 through December 2018. Only patients with post-procedural MRI (in tandem with pre-procedural MRI, per standard protocol) were included. Procedural times and number of passes attempted were recorded, and infarct volume on MRI was measured using region-of-interest analysis. MRI infarct growth was evaluated using linear regression analysis as a function of procedural duration and number of passes.
Of 173 patients who underwent mechanical thrombectomy over the three-year period, 118 had a post-procedure MRI study and were included in the analysis. Recanalization was successful (TICI score > 2b) in 106 of the 118 patients (89.8%).
Analysis revealed the following:
Advertisement
“In addition to finding that infarct growth was time-dependent, we saw that once you go beyond three attempted passes, infarct growth increases dramatically,” says Dr. Hussain. “This suggests that a fourth attempt seems to be a sort of crossing point where risk to the patient may outweigh potential benefit and further attempts at mechanical thrombectomy may not be justified.”
He notes that this finding is consistent with prior studies showing that patient outcomes correlate with time to recanalization, with outcomes starting to notably decline after 60 minutes and dropping precipitously after 90 minutes. “If you’re attempting three passes, you’re probably getting close to that 60-minute mark,” he observes.
Dr. Hussain’s team presented a related abstract from the same cohort of ELVO patients at ISC 2020, this time focusing on MRI infarct growth according to timing of mechanical thrombectomy.
Of 117 patients from the cohort who met inclusion criteria, 40 (34.2%) underwent early intervention (arterial puncture within 6 hours of ELVO onset) and 77 (65.8%) underwent late intervention (arterial puncture between 6 and 24 hours after ELVO onset).
Analysis showed that patients in the early intervention group demonstrated a trend toward less infarct volume growth versus those in the late intervention group (16.0 ± 42.9 mL vs. 31.4 ± 60.9 mL; P = 0.16). Ratios of pre- to post-intervention infarct volume were significantly different between the early and late interventions groups (P = 0.02), indicating less infarct growth in the early group. “A substantial number of patients in the early window had diffusion-weighted imaging [DWI] reversal,” Dr. Hussain notes.
Advertisement
“These results were a bit surprising, as we had expected patients in the later treatment window to have less infarct growth due to the likelihood that they had better collateral vessels,” he continues. “DWI reversal seems to have contributed substantially to the final infarct volumes in the early time window. While DWI has been thought to represent final infarct, we should reexamine this theory in the early time window.”
Studies like these represent the evolving research needs around mechanical thrombectomy and ELVO, Dr. Hussain adds. “Now that mechanical thrombectomy is established as a standard of care for ELVO, the relevant research questions include which patients may benefit from this therapy beyond those who fell within the clinical trials’ narrow inclusion criteria,” he says.
“Studies like these analyses of infarct growth help us refine how we perform the procedure and improve patient selection,” he observes. “We will continue to evaluate questions like these to ensure we’re not missing any patients who can benefit from this therapy.”
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges