One way colorectal surgeons can assist in the crisis
By Amy Lightner, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Like most of my fellow colorectal surgeons, I haven’t managed Acute Respiratory Distress Syndrome (ARDS), the most common complication of COVID-19, since residency. Some of us will undoubtedly be called to brush up on our skills and assist in the ICU, but our extensive experience with mesenchymal stem cells (MSCs) may help a broad swath of COVID-19 patients, even if we are not called to manage a ventilator. I recently published an article on how we might apply our knowledge of MSCs to help with COVID-19 in Diseases of the Colon and Rectumwith my fellow surgeon from Madrid, Damian Garcia-Olmo, PhD.
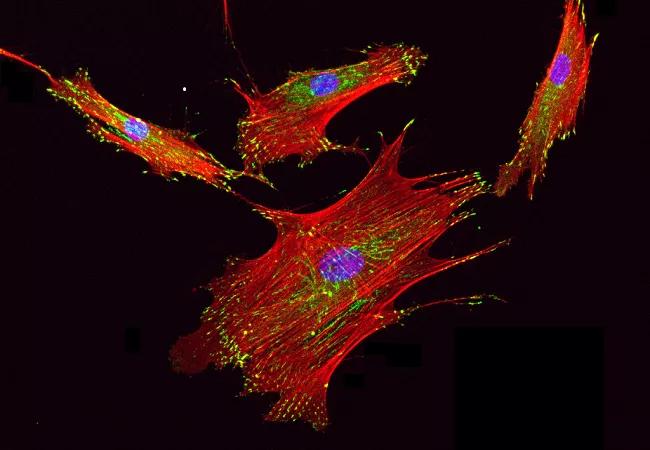
MSCs have demonstrated efficacy and safety in several clinical trials as a potent immunomodulatory and anti-inflammatory agent. These cells have been shown to shift the immune response from Th1 to Th2 and promote B-cell migration. Toll-like receptors, which have been linked to inflammatory diseases like Crohn’s, can modulate MSC behavior. In a murine sepsis model, adipose-derived MSCs decreased proinflammatory mediators TNF-α, IL-6, IL-1b, IL-12 and interferon-gamma and increased iL-10 in the main affected organs, among other anti-inflammatory and immunomodulatory effects. Several studies have demonstrated that adipose-derived MSCs get trapped in the lung upon intravenous administration.
Based on these and other data, MSCs have been used to treat complex fistula in patients with Crohn’s disease. Many of us who treat digestive diseases have witnessed the repair and regeneration of damaged tissue with local administration of MSCs. It appears COVID-19 patients are benefitting as well.
Advertisement
Like patients with Crohn’s, patients with COVID-19 experience hyperinflammation with a cytokine storm, thus creating an increase in lung endothelial and epithelial permeability and leading to ARDS. Once a patient with COVID-19 has ARDS, the mortality rate can hit 40%, despite treatment with antivirals, immunoglobulins, ventilation and glucocorticoids.
Both preclinical and clinical studies indicate that MSCs enter the lungs and release anti-inflammatory factors, reducing cytokine proliferation and modulating T-cells and macrophages to bring down inflammation. Two studies of a total of eight patients from China demonstrate that this process has potential to increase survival for COVID-19 patients with ARDS. All eight patients were extubated within days of MSC intravenous infusion and subsequently discharged from the hospital.
Four more clinical trials in China are enrolling. MSC-producing companies across the globe are working on Phase III clinical trials and emergent use and compassionate use cases.
We don’t know for sure if MSCs work for patients with COVID-19-related ARDS. But we have a significant amount of data demonstrating the safety of this therapy in humans, and these are unprecedented circumstances. If intravenous MSCs work for half of ventilated patients, that’s a significant win. As colorectal surgeons and gastroenterologists, we have extensive knowledge of utilizing these therapies in our patients with Crohn’s disease. We have an opportunity to apply what we have learned to alternative pathologies and play a significant role in the fight against COVID-19.
Advertisement
Dr. Lightner is a surgeon and Associate Chief of Surgical Research in the Department of Colorectal Surgery in Cleveland Clinic’s Digestive Disease & Surgical Institute.
Advertisement
Advertisement

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition

As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19