Sheath, endoscope size matter in percutaneous nephrolithotomy
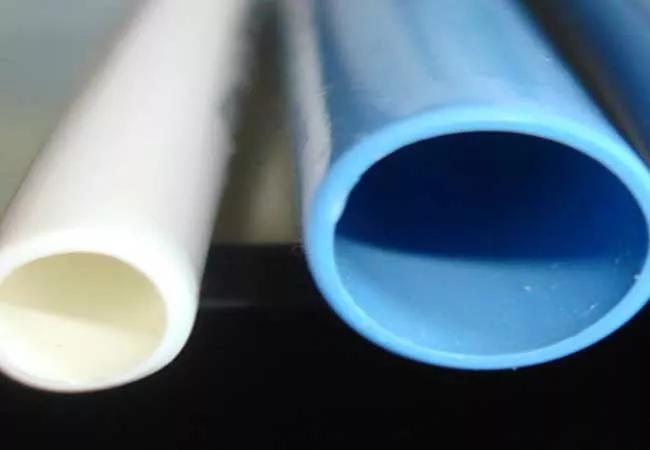
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d96947ee-b633-496e-8260-a62a791f3100/650x450-Monga-PCNL_jpg)
650×450-Monga-PCNL
A Cleveland Clinic study comparing two percutaneous nephrolithotomy (PCNL) methods confirmed size does matter when it comes to sheath and endoscope.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
PCNL is the standard of care for managing large kidney stones, but it carries complication rates of close to 15 percent. Major complications include bleeding, fever, pyelonephritis, systemic inflammatory response syndrome (reported at up to 28 percent) and sepsis (resulting in the deaths of four in 1,000 patients).
Knowing that high pressure in the kidney increases the risk of sepsis, Manoj Monga, MD, FACS, FRCS, Director, Cleveland Clinic’s Center of Endourology & Stone Disease in the Glickman Urological & Kidney Institute, and his team evaluated how sheath and endoscope size affect intrarenal pelvic pressure and the risk of postoperative infectious complications. Their study was published in the Journal of Endourology.
The team compared “mini” vs. “standard” PCNL using simulated PCNL surgeries in a porcine model of an infected urinary system using one strain of uropathogenic E. coli. The study tested the theory that mini-PCNL elevated renal pelvic pressures and impacted infectious indicators.
The study validates concerns that small sheath and endoscope size may lead to adverse outcomes after PCNL due to higher intrarenal pressures. Mini-PCNL was associated with higher intrarenal pressures and higher risk of end organ bacterial seeding in the setting of an infected collecting system. This can lead to a potentially higher risk of infectious complications.
Although not statistically significant, the mini arm demonstrated that blood cultures were positive for uropathogenic E. coli, which was attributed to the large amount of time spent at high pelvic pressures.
Advertisement
“This is the first study to culture the spleen and liver in the scenario of high intrarenal pressures in an infected kidney,” Dr. Monga says. “I was surprised by the high level of positive cultures in these organs.”
He says the study should serve as a warning to urologists.
“Approach the utilization of mini-PCNL with caution, especially in those patients who are at risk for sepsis,” Dr. Monga cautions.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key