By Yasser Rodriguez, MD, MBA, Cardiac Pacing and Electrophysiology, Cleveland Clinic Weston Hospital
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is reprinted from Cardiac Care Publication News From Cleveland Clinic in Florida.
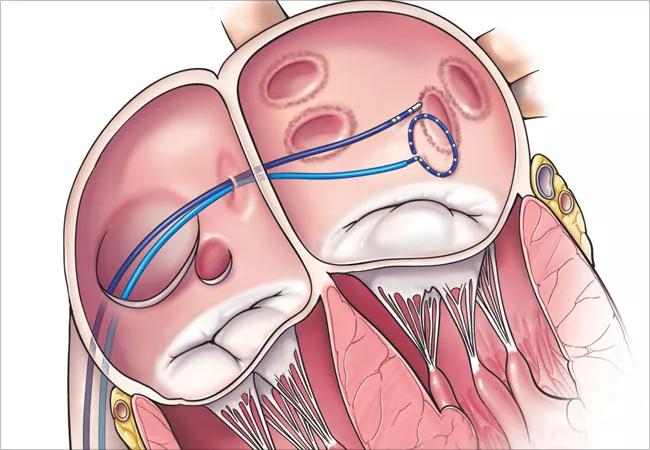
Catheter ablation procedures for cardiac arrhythmias were first undertaken in the 1970s and 1980s. Traditionally, these procedures required the use of ionizing radiation (fluoroscopy or continuous X-rays) to visualize the catheters in the heart (Image 1). Patients could receive anywhere from 9.5 – 41 minutes of continuous radiation, or the equivalent of 830 chest X-rays during a single ablation. Exposure to such radiation has been linked to the prevalence of malignancy later in life (Image 2).
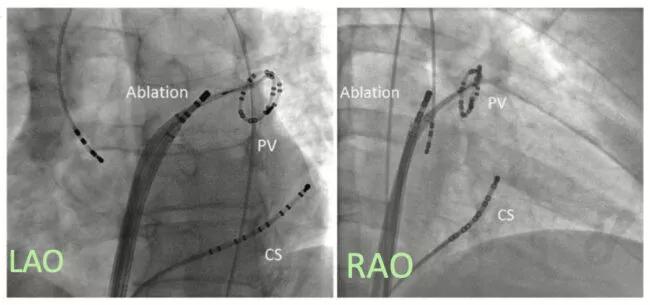
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/226879c7-cb90-48ef-9494-396fda57e6b6/Image-1-Fluoroscopy-650x305-1_jpg)
Image 1 (Left), Image 2 (Right)
The role of cardiac ablation as a treatment option continues to increase gradually with improving technology and techniques and changing demographics. Age is the most common risk factor for the development of certain cardiac arrhythmias. The prevalence of arrhythmias such as atrial fibrillation (AF) has increased three-fold in the past 50 years, and it is projected that anywhere from 6 to 16 million individuals will develop AF by the year 2050. These changes place an increased importance on the development of safer, more efficient and effective workflows to perform cardiac ablations.
Advances in technology have facilitated the elimination of fluoroscopy in cutting edge approaches to ablation, thus ushering in the era of “zero-fluoroscopy ablations.” Rather than traditional reliance on radiation to position cardiac catheters, a combination of intracardiac ultrasound (ICE; Image 3) and electroanatomic mapping (EAM; Image 4) is used to perform these procedures. The two modalities are further combined with tactile feedback to enhance the safety of the procedure. The use of intracardiac echocardiography allows for continuous, real time monitoring throughout the entirety of the procedure in addition to an overall enhancement of the safety of the ablation.
Advertisement
Zero-fluoroscopy ablations also have ushered in a drastic reduction in the length of the procedure. Traditionally, ablations could take as long as 4 to 6 hours, and require a brief hospitalization. At Cleveland Clinic Weston Hospital, these procedure times have been drastically reduced to 45 to 60 minutes, and patients are often discharged the same day.
Historically, zero-fluoroscopy ablation workflows were created targeting ablations for atrial fibrillation – the most common arrhythmia affecting the U.S. population. However, workflows have been created and adopted for other arrhythmias such as supra ventricular tachycardia, ventricular tachycardia, and atrial flutter. Multiple studies have demonstrated comparable or improved safety and efficacy for these “fluoroless” approaches.
“Fluoroless” ablations have emerged as a safe option with no increase in complication rates when compared to the traditional approach. At Cleveland Clinic, we have paired this approach with force-sensing and ablation indexes for improved patient outcomes and results. Ablation indexes are measures of the quality of the lesions we apply during a radiofrequency ablation, and superior values have been linked to improved long-term results for the patient. Ablations have evolved into an effective and safe tool in the management of cardiac arrhythmias. Ultimately, the most effective management strategies require a multi-disciplinary approach. Consultation with an electrophysiologist early in the diagnosis of cardiac arrhythmias is preferred and ultimately leads to better patient care and improved outcomes.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.