Distribution is beginning, but there are questions about effectiveness, supply and adverse events
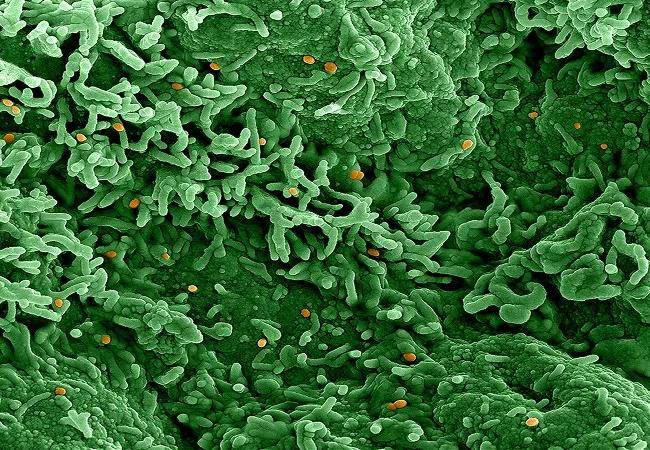
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fdb5dc05-a004-4200-b9fb-de8cf1f6c607/22-CCC-3109770-Monkeypox-virus-NIAID-650x450-1-jpg)
MONKEY_POX_22-CCC-3115237_radigan
Editor’s Note: In November 2022, the World Health Organization and the U.S. Centers for Disease Control and Prevention renamed the monkeypox virus “mpox.” We have updated some language in this article to reflect that change (although not in contemporaneous quotes or references to previously conducted studies), and will use mpox in new articles relating to the virus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The good news: Smallpox vaccines, particularly second- and third-generation versions, provide some protection against the rapidly spreading and genetically related mpox virus.
But uncertainties about the extent of the vaccines’ effectiveness, the potential for adverse reactions, manufacturing and distribution issues, the limited amounts of currently stockpiled reserves, and the wariness of a COVID-weary public toward more shots all pose considerable challenges to controlling the global mpox outbreak.
Current public health strategies to prevent or lessen illness involve vaccinating people after known mpox exposure and prophylactically inoculating members of at-risk populations presumed to have been exposed to the virus in some urban areas where mpox case levels are high. Mass public vaccination campaigns are not currently under consideration in the United States.
“Right now, monkeypox doesn’t seem like it’s going to be hugely severe, but we don’t know what happens when you get millions of cases,” potentially overwhelming hospitals, says Ted M. Ross, PhD, Cleveland Clinic’s Global Director of Vaccine Development and an eminent virologist and immunologist. “You can easily see monkeypox becoming endemic until the vast majority of the U.S. population is immune. We’re about at the point where we’ve missed the opportunity to be able to stop that from happening. We just can’t vaccinate people fast enough or get them aware fast enough.”
Dr. Ross, Jae Jung, PhD, Director of Cleveland Clinic’s Global Center for Pathogen & Human Health Research, and their colleagues are discussing projects to conduct surveillance for mpox infection in patient populations, develop a rapid clinical test and collaborate on a new mRNA- or protein-based mpox vaccine. Dr. Jung’s lab is conducting research that may lead to new mpox therapeutics.
Advertisement
Mpox has been endemic in central and western Africa for decades, with periodic outbreaks — and subsequently increased public health concerns — in other parts of the world, including clusters of cases in the United States in 2003 and in the United Kingdom and Israel in 2018.
The current and most extensive transmission event began in May 2022 and now constitutes more than 17,000 confirmed cases in 82 countries, including more than 2,800 cases in the United States. Those figures are likely an undercount. A recent survey of more than 8,200 cases in the European region shows most involve young men, many of whom are HIV-positive. Gay and bisexual men with multiple male sex partners are considered to be at elevated risk for mpox infection.
On July 23 the World Health Organization (WHO) declared the global spread of monkeypox a Public Health Emergency of International Concern, its highest alert level, despite its advisory committee’s failure to reach a consensus on whether the action was warranted. Some public health experts previously had labelled the outbreak a pandemic and called for more extensive public education, testing and targeted vaccination efforts. The WHO’s decision may increase pressure on member states to take steps to respond.
The causative agent of mpox is a zoonotic double-stranded DNA virus belonging to the Orthopoxvirus genus, which also contains the Variola major virus, the causative agent of smallpox.
Mpox’s clinical features — fever, chills, headache, lethargy, lymphadenopathy, myalgia and a body-wide rash progressing from macules to pustules — are very similar to those of smallpox, although mpox has a lower mortality rate (1%-10% versus ~30%) and is less contagious. The course of the disease can be more severe in children and immunocompromised patients. Following infection, incubation can take from 5 to 21 days. Symptoms last 2 to 4 weeks.
Advertisement
Mpox was first identified in monkeys in 1958 and in humans in 1970. Despite its original name, the virus is not confined to primates; the extent of its natural reservoir in host animals is unknown but it has been detected extensively in rodent populations including squirrels, rats and mice.
Animal-to-human transmission is thought to occur via direct (bites, scratches) or indirect contact with live or dead animals, with consumption of inadequately cooked meat a potential risk. The precise method of human-to-human infection is uncertain but presumably occurs through inhalation of large respiratory droplets, or direct or indirect contact with body fluids, lesions, or recently contaminated materials such as clothes or bedding. Transplacental infection from mother to fetus is possible. It is currently unknown whether the virus is transmissible via semen or vaginal fluids, but limiting the number of sex partners may reduce exposure risk.
“The virus has been found in semen and saliva,” Dr. Ross says. “It’s not clear if monkeypox is sexually transmitted or the virus is just able to spread through skin-to-skin contact or by getting it into the eyes, nose or mouth in a way that would cause transmission.”
“Most people infected with monkeypox will have a mild disease course,” he says. “There is probably a large pool of people who are infected and don’t realize it because they have minor symptoms and only one or two skin lesions. The disease is uncomfortable but typically does not require hospitalization, although its progression hasn’t been extensively explored in patients who are immunologically suppressed or have comorbidities. Monkeypox is self-limiting; people who have been infected are immune to re-infection.”
Advertisement
Because of the close genetic relationship between mpox virus and the variola virus, the first-generation live vaccinia-based smallpox vaccines that were widely distributed from the 1950s through the 1970s as part of an ultimately successful global smallpox eradication effort provided some cross-protection against mpox, according to experimental studies conducted in chimpanzees in the 1960s. Routine smallpox vaccination of the American public ended in 1972 after the disease was eradicated in the United States. Vaccination campaigns in other countries were discontinued after the global eradication of smallpox was certified in December 1979.
The degree and duration of mpox cross-protection in people who received the original smallpox vaccinations is uncertain, although a 1988 study of monkeypox infection rates in Zaire residents indicated that smallpox vaccination prior to its 1980 discontinuation in that country conferred approximately 85% protection against monkeypox at the time the research was conducted. The researchers predicted that vaccine-derived protection from monkeypox would decline over time.
“If you are on the younger end of those who received the original smallpox vaccine, I would like to think you are going to have a level of protection that might prevent monkeypox infection and spread,” Dr. Ross says. “But as we age, our immune system begins to wane, so some of the people over 70 or 80 years old may no longer retain those antibodies at high enough levels to prevent infection.”
Advertisement
To determine the extent of remaining cross-protection in the original vaccine cohort, “we would need to conduct prevalence studies to know whether people in different age groups are getting infected with monkeypox,” Dr. Ross says. “We would also need to do serology collection to see if people have antibodies to smallpox, and controlled studies to see if those smallpox antibodies actually neutralize monkeypox virus in tissue culture. I don’t think that’s been done at the population level.”
Nearly half of the current U.S. population was born after routine smallpox vaccination was halted in this country, meaning they lack adaptive immunity to smallpox or, by extension, mpox. Because of their unvaccinated status, “teens, 20- and 30-year-olds are probably the most susceptible population to monkeypox,” Dr. Ross says. “It’s not surprising that you’re seeing it among sexually active individuals, particularly in urban settings.”
Manufacturing of the original smallpox vaccine stopped in 1978 with the disease’s impending eradication. Following the Sept. 11, 2001, terrorist attacks, the United States and other governments began reconstituting vaccine stockpiles, including smallpox, due to bioterrorism concerns. Production of second- and eventually third-generation smallpox vaccines began.
U.S. stockpiles currently contain the second-generation ACAM2000 and third-generation JYNNEOS™ smallpox vaccines. When properly administered before exposure, both vaccines are capable of providing immunity against mpox, according to the U.S. Centers for Disease Control and Prevention (CDC). Post-exposure vaccination (within 4 to 14 days) may help prevent mpox infection or reduce its severity.
ACAM2000 is a live Vaccinia virus single-dose vaccine licensed by the U.S. Food and Drug Administration (FDA) in 2007 for smallpox prevention. Full immunity is achieved 4 weeks after vaccination. The FDA’s expanded access investigational new drug protocol allows ACAM2000 to be used for mpox immunization during an outbreak.
ACAM2000’s immunogenicity and protective efficacy were determined to be equivalent to the first-generation smallpox vaccine Dryvax® using both animal and human subjects. Cohorts of cynomolgus macaques vaccinated with ACAM2000 or Dryvax and subsequently given a lethal intravenous dose of mpox virus each showed no evidence of viral replication or clinical signs of monkeypox infection. In a double-blind human clinical study, ACAM2000 and Dryvax were equal in their ability to produce major cutaneous reactions (a localized infection site or “take”) and to induce neutralizing antibody and cell-mediated immunity against Vaccinia virus.
Because ACAM2000’s Vaccinia virus component can replicate, inadvertent spread of the virus from the vaccination site to other areas of the body or to other individuals is possible, necessitating precautions.
ACAM2000 also may cause serious adverse events — specifically, myocarditis and pericarditis. It is contraindicated in people with underlying heart disease or three or more major cardiac risk factors; women who are pregnant or breastfeeding; infants younger than 1 year; people with severe vaccine component allergies; immunosuppressed patients; and people with atopic dermatitis or other active exfoliative skin conditions.
Those issues raise questions about ACAM2000’s suitability for mass vaccinations, whether for smallpox or mpox, although it continues to be maintained in the federal government’s Strategic National Stockpile (SNS) as the predominant vaccine for those diseases. One estimate determined that 25% of the general population would be at risk of developing complications if administered first- or second-generation smallpox vaccines such as ACAM2000.
Seeking a safer alternative, the U.S. government has added the third-generation smallpox vaccine JYNNEOS (also known as MVA-BN, or modified vaccinia Ankara-Bavarian Nordic) to the SNS. JYNNEOS was licensed by the FDA in 2019 for prevention of both smallpox and monkeypox in adults — the first dual-use vaccine for those diseases. An expanded-access protocol authorizing pediatric administration of JYNNEOS for mpox protection is being developed.
JYNNEOS utilizes a live, attenuated, nonreplicating vaccinia variant delivered in two subcutaneous injections four weeks apart. Full immunity is achieved 2 weeks after the second dose. Because the viral component is replication-deficient, inadvertent inoculation is impossible, as is clinical infection. Thus, JYNNEOS poses a substantially lower risk of adverse events compared to ACAM2000. However, the CDC says that because the mechanism for myopericarditis following ACAM2000 vaccination is thought to be an immune-mediated phenomenon, it is unknown whether the antigen(s) that precipitate autoantibodies are also present in JYNNEOS.
JYNNEOS’ effectiveness against smallpox and mpox is inferred from its immunogenicity in clinical studies and from efficacy data from animal challenge studies. In the latter, cynomolgus macaques were administered either ACAM2000 or JYNNEOS followed by an aerosolized lethal dose of mpox virus. A single JYNNEOS dose did not protect all of the animals in the cohort, but the recommended two-dose regimen provided complete protection, comparable to the results in the ACAM2000-vaccinated monkeys.
The CDC says no data are available yet on the effectiveness of ACAM2000 and JYNNEOS in the current mpox outbreak.
As of late June, the SNS held more than 100 million doses of ACAM2000 and approximately 65,000 doses of JYNNEOS in its immediate inventory. On June 28, the U.S. Department of Health and Human Services (HHS) announced it would distribute 56,000 doses of JYNNEOS from the SNS to states and territories for vaccination of at-risk populations, prioritizing jurisdictions with the highest number of cases and population at risk.
Previously, vaccines had only been provided for cases of known mpox exposure, but the new HHS policy calls for vaccination of individuals with confirmed and presumed exposures, including:
In the next few weeks, HHS expects to receive an additional 240,000 doses of JYNNEOS from the vaccines’ manufacturer, Denmark-based Bavarian Nordic, allowing vaccination of a broader population of at-risk individuals. HHS officials say more than 750,000 JYNNEOS doses will be made available over the summer. An additional 500,000 bulk doses will undergo completion, expedited inspection and release throughout the fall, totaling 1.6 million JYNNEOS doses available this year. HHS anticipates distributing a total of more than 4 million JYNNEOS in 2022 and 2023.
States and territories also can request allocation of ACAM2000 vaccines, but not for distribution to people to who are immunocompromised or who have heart disease.
While states with sizeable populations and/or large urban areas have requested large allocations of JYNNEOS vaccine, others have not. “Most places in the U.S. aren’t putting this on their radar yet,” Dr. Ross says. “It might take more to get their attention.”
Some public health experts have raised concerns about the limited supply of JYNNEOS available initially, about the United States relying on a single vaccine manufacturer, and whether vaccines will be available in other parts of the world, especially in Africa where mpox is endemic.
“The reason COVID vaccines were out so quickly is because there was a huge government push and they were helping to subsidize the development, production and the distribution,” Dr. Ross says. “If it falls on just one company to make hundreds of millions of doses for the world, that’s going to be very expensive. Science is important in the rollout of a vaccine, but economics plays a huge part.”
The SNS also contains more than 1.7 million treatment courses of the smallpox antiviral drug Tecovirimat (also known as TPOXX), whose expanded-access investigational new drug protocol also allows its use to treat mpox. Potential recipients include:
The limited supply of TPOXX means most patients infected with mpox will receive palliative care, Dr. Ross says.
In late June, the CDC began shipping an FDA-cleared orthopoxvirus test to five major commercial laboratory companies to rapidly increase mpox testing. The CDC also published the FDA-approved testing protocol so that other laboratories could begin testing for mpox, and the FDA has allowed hospitals to develop their own high-quality mpox tests.
At Cleveland Clinic, a team in Dr. Jung’s lab led by Grace Lee, MD, has been working to better understand how orthopoxviruses, including mpox, evade the immune system. The team is examining the role of the small viral protein E3, encoded by the E3L gene. E3 is conserved among poxviruses and inhibits necroptosis, thus helping counteract host innate immunity. Their findings may aid efforts to develop new therapies.
Drs. Ross, Jung and others at the Global Center for Pathogen & Human Health Research have had preliminary conversations about additional ways to help combat mpox. Those efforts could include:
Advertisement
First full characterization of kidney microbiome unlocks potential to prevent kidney stones
Researchers identify potential path to retaining chemo sensitivity
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time
Investigators are developing a deep learning model to predict health outcomes in ICUs.
Preclinical work promises large-scale data with minimal bias to inform development of clinical tests
Cleveland Clinic researchers pursue answers on basic science and clinical fronts
Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches
Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology