Pairing of novel imaging technique with post-processing analyses could ultimately reshape care
Researchers at Cleveland Clinic and Case Western Reserve University in Cleveland have received a $3 million, five-year R01 grant from the National Institutes of Health (NIH) to use a novel imaging method known as magnetic resonance (MR) fingerprinting to quantitatively assess brain pathology to improve epilepsy care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The award supports application of the MR fingerprinting technology for use in patients with epilepsy by experts from Cleveland Clinic’s Epilepsy Center. “We will be using computer post-processing of the MR fingerprinting images, a strategy that our Epilepsy Center has already used successfully with conventional MRI,” says Cleveland Clinic staff scientist Irene Wang, PhD, who is co-principal investigator on the grant along with Dan Ma, PhD, of Case Western Reserve University.
“Our goal is to further develop machine learning algorithms to analyze the images and thereby improve diagnosis in challenging epilepsy cases,” Dr. Wang continues. “We believe this combination of innovations will allow visualization of small, subtle epileptic pathologies that we could not see before. This will aid identification of candidates for epilepsy surgery and help pinpoint where in the brain their seizures originate.”
An example is provided in the images below.
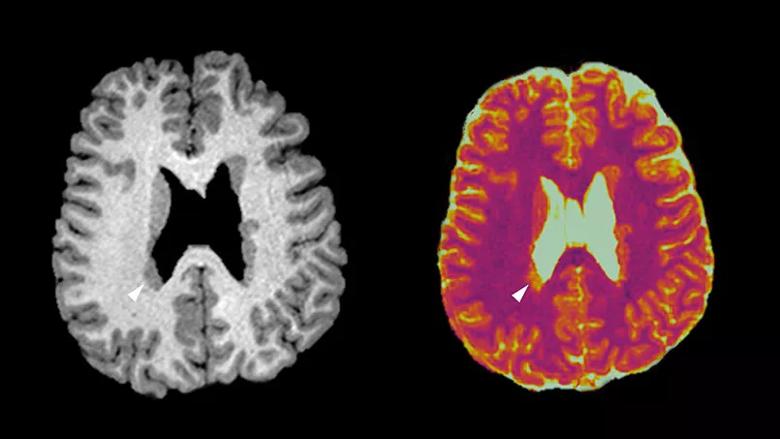
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/46998d0b-c0f6-460c-8439-6eab8405c271/805x-Inset-Wang-NIH-grant_jpg)
Sample images from a patient with right temporoparietal epilepsy in whom MR fingerprinting (right) was able to differentiate active from nonactive periventricular nodular heterotopia lesions when conventional T1-weighted MRI (left) was not. Whereas the conventional MRI shows uniform signal intensity of the bilateral nodules, MR fingerprinting shows distinct T1 signal increase in the nodules at the posterior part of the right lateral ventricle. These nodules were later confirmed to be the seizure onset zone by intracranial EEG monitoring. Images shown with radiological convention.
Dr. Wang notes that promising pilot data from this translational work was recently published in the Journal of Magnetic Resonance Imaging (2019;49:1333-1346), helping to pave the way for the work to be undertaken under the NIH grant.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help