New Lancet review brings specialists, generalists up to speed
“We’re making headway in the understanding of progressive multiple sclerosis and starting to change the traditional attitude that it’s untreatable.” So says Cleveland Clinic neurologist Daniel Ontaneda, MD, MSc, in recapping an invited review of progressive multiple sclerosis (MS) he recently co-authored for The Lancet (2016 Nov 23 [Epub ahead of print]).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The paper’s goal was to update a general medical audience on current knowledge of progressive MS, the form of the disease during which disability accrues the most — and which has largely proved resistant to therapy to date. Key takeaways from the review — which Dr. Ontaneda drafted with his colleagues Robert Fox, MD, and Jeffrey Cohen, MD, from Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, along with Alan Thompson, MD, of University College London — are outlined below.
In recent years, scientists have gained a better understanding of the underlying differences between progressive MS and relapsing-remitting MS, the latter of which typically characterizes the first 10 to 15 years of a patient’s disease course.
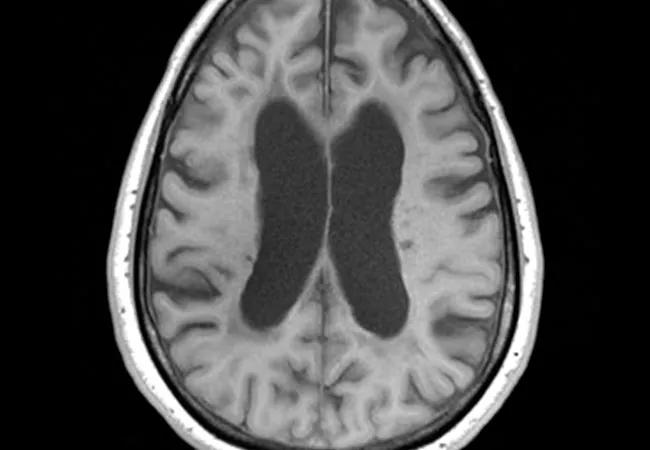
While relapsing-remitting MS generally involves focal inflammatory lesions, demyelination and periodic clinical relapses, progressive MS is characterized by more diffuse mechanisms, involvement of normal-appearing white and gray matter, and more prominent neurodegeneration affecting long-term brain function. The physiological processes elucidated by recent research in progressive MS provide important new targets for potential therapies.
The phenotypic categories of progressive MS have been revised based on increasing recognition that progressive disease sometimes involves relapses and MRI-apparent lesion activity similar to what is seen in relapsing-remitting disease.
Like the older classification system, the new scheme differentiates between primary disease (progression at disease onset) and secondary disease (progression after a relapsing-remitting course) but also factors in clinical relapses, new MRI lesions and worsening disability.
Advertisement
The authors emphasize that categories are not meant to be regarded as static entities, since patients’ signs and symptoms may change during the course of their disease. The new system is expected to be especially useful for standardizing participant selection for clinical trials.
Standard MRI has limited utility for assessing progressive MS: Unlike in relapsing-remitting MS, visible lesion activity is uncommon and does not correlate with disability. MRI markers have been enormously helpful in assessing treatment effectiveness in clinical trials for relapsing-remitting MS, but tools of this type are lacking for progressive disease.
Scientists are now exploring the utility of new imaging modalities and approaches to meet this need. The review describes a number that show promise:
Fourteen anti-inflammatory drugs have been approved for the treatment of relapsing-remitting MS, but they have largely proven ineffective for progressive disease.
A notable exception is ocrelizumab, a humanized monoclonal antibody that selectively depletes CD20-expressing B cells. It was recently shown in the phase 3 ORATORIO trial to reduce confirmed disability worsening in primary progressive MS by 24 percent relative to placebo; MRI progression was also significantly reduced with active treatment. The trial followed 488 patients on ocrelizumab and 288 patients taking placebo for 120 weeks, but extended observation is needed to determine long-term safety and efficacy.
Advertisement
Additional strategies are also being explored to tackle progressive MS. One approach that has shown initial promise is high-dose biotin (300 mg/d), which was found in the French MS-SPI study to improve MS-related disability in a subset of patients over 12-month period. This vitamin is believed to enhance cellular energy production, resulting in improved axonal function, decreased neurodegeneration and enhanced remyelination.
Cell-based repair-promoting strategies are also being investigated, including the use of oligodendrocyte progenitor cells as the basis for high-throughput screening of drugs for their ability to stimulate remyelination. Mesenchymal stem cell transplantation to directly promote tissue repair is also being studied.
“We now have a much better understanding of how progressive MS is different in fundamental ways from the relapsing-remitting form and therefore cannot be treated in the same way,” observes Dr. Ontaneda. “This knowledge encourages researchers to take investigations in new directions, which we are hopeful will lead to effective treatments.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help