SARS-CoV-2’s potential for neuroinvasion and primary emerging neurologic features
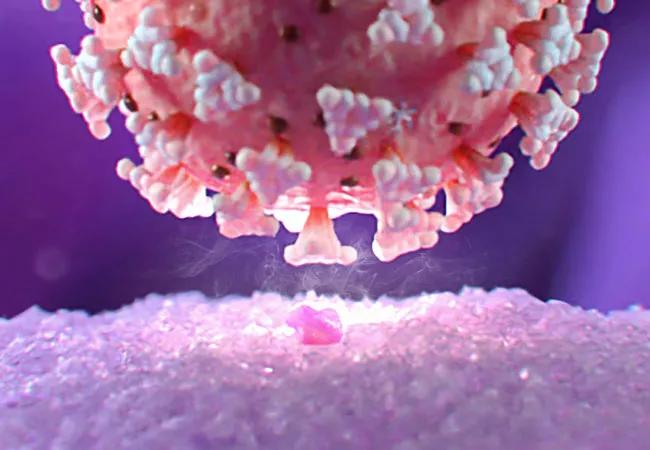
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/da7f1044-befc-41f6-a929-b038eeaca606/20-NEU-1882828_SARS-CoV-2-microvillie_650x450_jpg)
20-NEU-1882828_SARS-CoV-2-microvillie_650x450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As reports of COVID-19 case series from China and elsewhere start to accumulate, we are getting a clearer picture of how infection with the virus known as SARS-CoV-2 can manifest in the brain and central nervous system (CNS). This brief report distills what is known to date in this fast-evolving realm.
In the earlier SARS and MERS outbreaks resulting from similar coronaviruses, neurological complications were reported in rare cases, typically developing two to three weeks into the course of the infection. These included axonal peripheral neuropathy and rhabdomyolysis (both likely related to critical illness neuromuscular syndromes), acute disseminated encephalomyelitis, Bickerstaff encephalitis/Guillain-Barré syndrome and large-vessel stroke.1-5
There are echoes of these complications in the neurologic manifestations of COVID-19 reported to date.
The most comprehensive picture so far comes from a retrospective chart review by Mao and colleagues of 214 consecutive patients in Wuhan, China, hospitalized for either severe (41.1%) or nonsevere (58.9%) COVID-19.6Patients in this series had risk factors similar to those in other COVID-19 reports. Notably, 78 of the 214 patients (36.4%) were reported to have neurologic manifestations, and these manifestations occurred in 45.5% of patients with severe COVID-19 versus only 30.2% of patients with nonsevere disease.
When data from this report of Mao et al6 are combined with findings from other COVID-19 reports to date,7-11 the leading neurologic manifestations break down as follows, with rough incidence rates in parentheses:
Advertisement
There have also been several rarer neurologic effects reported across these collective reports, including neuralgia (2%), ataxia (0.5%), seizures (0.5%), acute hemorrhagic necrotizing encephalopathy (1 case), Guillain-Barré syndrome (1 case) and acute disseminated encephalomyelitis (anecdotal reports).
[Editor’s note: Since this article was written, researchers from three hospitals in northern Italy reported five cases of Guillain-Barré syndrome that developed in association with COVID-19. These cases occurred within a three-week period when there were an estimated 1,000 to 1,200 COVID-19 admissions to these hospitals. The first symptoms of the syndrome occurred within 5 to 10 days of the start of COVID-19 symptoms. For more, see the report: N Engl J Med. Published online April 17, 2020.]
Among the above potential manifestations, four particular neurologic features of COVID-19 are increasingly being noted and recognized as potentially more common than initially realized:
All of these manifestations can occur early in the course of COVID-19 and in either the presence or absence of other symptoms, arguing for a higher index of suspicion for SARS-CoV-2 infection when they are present without other explanation. Anosmia is notable in that it can develop acutely and may occur with or without nasal congestion.
Putative mechanisms of anosmia in this setting include nasal congestion, inflammatory obstruction of the nasal cleft and infection of the olfactory bulbs or CNS neurons.12 Proposed mechanisms of stroke include an overlap in vascular risk factors between stroke and COVID-19, the hypercoagulability observed in some patients with COVID-19, and theoretical deleterious effects of ACE inhibitor or angiotensin receptor blocker use related to binding of SARS-CoV-2 to the ACE2 receptor.6
Advertisement
Concern surrounding encephalopathy has been fueled by a recent report of a U.S. female airline worker in her late fifties who was hospitalized with a three-day history of fever, cough and altered mental status.10 RT-PCR testing for SARS-CoV-2 was positive. Cerebrospinal fluid (CSF) analysis was limited because of a traumatic lumbar puncture; while testing for SARS-CoV-2 in CSF could not be performed, other tests showed no evidence of other viral infections.
Brain MRI showed hemorrhagic rim-enhancing lesions primarily in the thalami and medial temporal lobes and also in the subinsular regions. This entity of acute hemorrhagic necrotizing encephalopathy has been seen in rare cases of other viral infections, including those caused by other coronaviruses and influenza virus. It is postulated to be an acute CNS demyelinating syndrome associated with the inflammatory cytokine release syndrome associated with infection with SARS-CoV-2 and other viruses.
There is concern that SARS-CoV-2 may be neuroinvasive, and that this may account for some of the neurologic manifestations of COVID-19 outlined above. Because neuroinvasive potential may have important implications for some disease-modifying therapies used for multiple sclerosis, this question has direct implications for neurologic clinical practice.13,14
Neurotropism has been seen among animal (PHEV) and human (SARS-CoV-1, MERS-CoV) coronaviruses, and because the coronaviruses share similar viral structure and infectious pathways, the pathophysiology of these viruses may be the same as that of SARS-CoV-2. Additionally, the ACE2 receptor (to which SARS-CoV-2 strongly binds) is expressed broadly by neurons in the brain, particularly in some brainstem centers involved in cardiorespiratory control. Medullary neuronal death has been proposed as a potential contributor to respiratory failure and other systemic manifestations of COVID-19.13,14
Advertisement
Several hypothetical routes for neuroinvasion have been postulated.15 One proposes direct entry from the oro/nasopharynx via the olfactory nerve or other cranial nerves, with subsequent spread from neuron to neuron throughout the CNS. Alternately, the virus may be carried into the brain by the blood, with subsequent infection of brain vascular endothelial cells or macrophages.
Advertisement
Dr. Cohen is Director of Experimental Therapeutics in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research and Director of the Clinical Neuroimmunology Fellowship in Cleveland Clinic’s Neurological Institute.
Advertisement
Patients report improved sense of smell and taste
Clinicians who are accustomed to uncertainty can do well by patients
Unique skin changes can occur after infection or vaccine
Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition
As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients
Early results suggest positive outcomes from COVID-19 PrEP treatment
Could the virus have caused the condition or triggered previously undiagnosed disease?
Five categories of cutaneous abnormalities are associated with COVID-19