Findings indicate clinical decision making should not be driven by initial lesion size

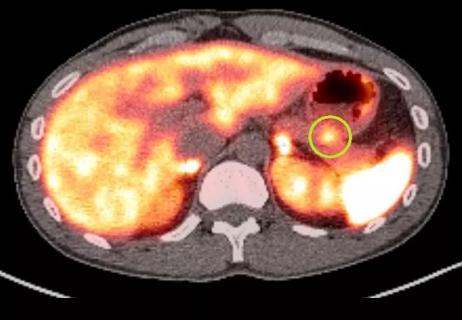
A recent analysis, led by Cleveland Clinic surgeon Matthew Walsh, MD, offers new insight into side-branch intraductal pancreatic mucinous neoplasms (SB-IPMNs) and the role of surveillance in clinical practice. Their findings — published in the journal Annals of Surgery — suggest that clinically relevant progression in these patients is uncommon and the development of cancer anywhere in the pancreas is rare.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Based on their research, the study authors conclude that decisions regarding surgical resection should not be driven by initial size. “Long-term and consistent non-operative surveillance is warranted, with surgery currently reserved for clinically relevant progression knowing that the majority of these still harbor low grade pathology,” says Dr. Walsh
Intraductal papillary mucinous neoplasms are cystic tumors of the pancreas that produce mucin. Previously, due to the risk of developing invasive cancer, discovery of any mucinous neoplasm prompted surgical resection. However, over time the approach to management of these patients has evolved.
While main-duct or mixed-type intraductal papillary mucinous neoplasms carry a significant risk of malignancy and typically require surgical intervention, side-branch IPMNs are acquired with increasing frequency as we age and are single or multiple cystic dilations of the peripheral branches off a normal main pancreatic duct and fortunately carry a lower malignancy risk.
“Many patients with side-branch intraductal papillary mucinous neoplasms are candidates for surveillance; however, SB-IPMNs are increasingly discovered incidentally, making it a challenge to determine which patients need resection,” notes Dr. Walsh. “Today, the majority of incidental lesions are surveilled, but the effects of this decision remain unclear. Our study sought to provide further clarity on SB-IPMNs and how to approach the management of these patients.”
In their analysis, which aimed to define the rate of progression during surveillance and determine when delayed resection is indicated, Dr. Walsh and colleagues used a prospectively maintained database of pancreatic cystic neoplasms to identify patients with side-branch IPMNs.
Advertisement
The study population included adult patients (> 18 years) who had at least two sets of cross-sectional abdominal imaging more than six months from diagnosis. Researchers defined clinically relevant progression (CR-Progression) by the following: symptoms, worrisome/high-risk stigmata or invasive cancer. Growth of more than 5 mm in two years is considered CR-Progression while a size of more than 3 cm alone is not, according to Dr. Walsh.
Between 1997-2023, an impressive total of 2,686 patients had a diagnosis of pancreatic cystic neoplasms of any type. Of these, 1,337 patients (49.7%) were diagnosed with suspected SB-IPMN. Thirty-seven (2.7%) patients received up-front surgery; 10 of these individuals (27.0%) had invasive cancer on surgical pathology and six (16.2%) had high-grade dysplasia (HGD). Three-hundred patients (22.5%) did not have adequate surveillance imaging.
One thousand patients (75%) received more than six months surveillance and were considered the study cohort, according to the investigators, who noted that the median cyst size at diagnosis in this surveillance cohort was 1.3 cm and the maximum size was 7 cm. Median age at diagnosis was 68.6 years. Additionally, 85 (8.5%) had a cyst size of more than 3 cm on initial imaging. The median imaging surveillance follow-up was 6.6 years.
Data showed a rate of CR-progression of 15.3% (n = 153) based on size increase (n = 63, 6.3%), main-duct involvement (n = 48, 4.8%), symptoms (n = 8, 5.0%) or other criteria (n = 34, 3.4%), according to Dr. Walsh and colleagues. The median time to clinically relevant progression was 3.4 years.
Advertisement
For patients with CR-progression, surgical resection was offered in 131 cases (85.6%) and 61 (39.2%) underwent surgery. Researchers reported that 28 patients (18.3%) with CR-progression had EUS-FNA with findings of high-risk dysplasia, which contributed to the indication for surgery.
At median follow-up of over 6 years, 17 surveilled patients (1.7%) developed invasive cancer. Among patients with CR- progression, 11.1% (n = 17) developed invasive cancer and high-grade dysplasia (HGD) was seen in 6.5% (n = 10). Dr. Walsh notes that almost half of the cancers were not contiguous with the surveilled side-branch intraductal papillary mucinous neoplasms.
The analysis also revealed that cysts with an initial size of more than 3 cm were not more likely to develop HGD/invasive cancer. Additionally, investigators found that cysts with CR-progressions determined by size growth (6.3%) were least likely to develop HGD/invasive cancer versus main-duct involvement (24%) or other non-size-based criteria (43%). Findings showed that size-based clinically relevant progression had the longest time without dysplastic transformation on time-to-event analysis (3.6 vs. 2.9 years).
Among the total cohort of surveyed SB-IPMN patients, surgical resection was not associated with improved overall survival when compared to those who did not undergo surgery. However, in patients with clinically relevant progression who received surgical resection, Dr. Walsh and team observed improved survival from the time CR-progression was detected.
Advertisement
“On multi-variate Cox-regression analysis in the total cohort, CR-Progression was the strongest negative predictor of overall survival from diagnosis followed by increasing age at diagnosis,” Dr. Walsh and colleagues note in their recent Annals of Surgery paper. “Pancreatic resection did not independently improve survival in the total population.
“In patients with CR-progression, the strongest predictor of reduced survival was invasive cancer. HGD, cyst size or type of CR-progression were not associated with decreased survival,” they explain. “However, pancreatic resection was independently associated with improved survival in this sub-cohort.”
Despite ongoing advancements, pancreatic cancer remains a devastating disease with a median survival of approximately two years and overall five-year survival rate of less than 5%. Consequently, patients and healthcare providers alike are eager to seize any opportunity to prevent pancreatic cancer by addressing precursor lesions promptly.
The work of Dr. Walsh and colleagues offers additional insights that can help inform clinical decision making for this patient population. To date, this is the largest study — with the longest follow-up — reporting surveillance for SB-IPMNs. Through their research, the investigators have defined a strategy for surveillance and potential resection of incidental side-branch intraductal papillary mucinous neoplasms. It is their recommendation to follow low-risk cysts with yearly scans for 10 years, or until evidence of clinically relevant progression.
Advertisement
Asked the take home message for his colleagues, Dr. Walsh concludes, “It’s important to have a balanced approach when it comes to decision-making for an operation that may be highly morbid. And, if you want to be a student of a disease, as a surgeon, understanding the outcome of people who aren’t getting surgery is equally as important as understanding the individuals who are.”
Advertisement

Patients spent less time in the hospital and no tumors were missed

A review of current evidence and recommendations
Patient’s unexplained low blood glucose levels in the absence of diabetes spark quest for answers
Pancreas and spleen removed to minimize risk of pancreatic cancer

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling