Online tool reveals characteristics that may increase recurrence risk

A Cleveland Clinic-led study has led to development of the first calculator that clinicians can use to evaluate the benefits and risks of post-mastectomy radiation therapy (PMRT) in women with early breast cancer. The tool and the data underpinning it will be presented at the 2020 American Society for Radiation Oncology (ASTRO) Annual Meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Up to this point, decisions about whether to treat pT1-2N1 disease with radiation therapy have been relatively subjective and controversial,” says Cleveland Clinic Cancer Center radiation oncologist Rahul Tendulkar, MD. “Our primary purpose was to provide objective data on a personalized level that clinicians and their patients can use to make individualized decisions.”
The evidence that powers the breast cancer outcome predictor comes from a study of 7,096 women who underwent mastectomy from 1995 to 2015 and were treated at five North American Institutions including Cleveland Clinic. All had stage pT1-2N1 breast cancer, one to three positive lymph nodes and no evidence of metastasis. None of the women had received neoadjuvant therapy.
To create the cohort, data from the institutions were collected retrospectively and pooled. A competing risk regression analysis was performed to identify factors associated with locoregional recurrence (LRR), distant metastases (DM), overall recurrence (OR) and breast cancer mortality (BCM).
LRR was defined as recurrent breast cancer in the ipsilateral chest wall, axilla, supraclavicular or internal mammary lymph nodes. All other sites of disease recurrence were considered distant metastases. OR was defined as either LRR or DM, whichever occurred first.
In patients who had received PMRT, the hazard ratio [HR] for LRR was 0.28 (95% confidence interval [CI] 0.21-0.37, P < 0.001). For DM, it was 0.79 (95% CI 0.69-0.91, P < 0.001) and for OR, it was 0.69 (95% CI 0.60-.79, P < 0.001). The HR for BCM was 0.81 (95% CI 0.69-0.94, P = 0.007).
Advertisement
“This is the largest series to date in this subgroup to look at factors associated with increased risk of recurrence,” says Sarah Sittenfeld, MD, radiation oncology resident and lead author of the study. “It showed a significant benefit favoring radiation therapy in terms of local, distant and overall recurrence, and also breast cancer mortality.”
Ten-year unadjusted cumulative incidence rates of LRR were 6.4% in the no PMRT group versus 2.6% in the PMRT group. There were no significant interactions between LRR and PMRT and number of positive nodes, tumor size, receptor status or N1mic versus N1.
Younger age (HR 1.03), larger tumor size (HR 1.25) grade III (HR 2.30), three positive lymph nodes (HR 1.60), higher nodal ratio (HR 1.75), lymphovascular invasion (LVI) (HR 1.55) and inner tumor location (HR 1.45) all were significantly associated with increased risk of LRR.
The clear-cut findings are noteworthy because of the controversy surrounding indications for PMRT in this stage of patients. Data from older randomized trials suggested that PMRT significantly reduces risk of LRR in women with one to three positive lymph nodes. But more recent studies have reported five-year recurrence rates ranging from 4% to 11% post-mastectomy in the absence of radiation therapy, suggesting that PMRT may not be needed in many of these patients.
“This study underscores the factors that are associated with higher risks of recurrence and identifies a subgroup of patients who might have a benefit that goes well beyond local control,” says Dr. Sittenfeld. “Most of the available studies to date have been small, single-institution studies, which individually lacked the statistical power and ability to give personalized risk estimates.”
Advertisement
Competing risk regression models for each primary endpoint included predictors defined a priori, including age, tumor size, grade, number of positive lymph nodes, ratio of positive lymph nodes to sampled lymph nodes, pathologic N stage, LVI, nodal extracapsular extension, estrogen receptor (ER) and progesterone receptor status, HER2/neu gene amplification and use of adjuvant contemporary chemotherapy and/or trastuzumab.
The primary model incorporated tests for interactions between PMRT and ER status, number of positive lymph nodes and pathologic N stage, and any significant interaction effects. After assessing the model’s discrimination and performing cross-validation, the prediction model was converted into an online calculator.
“The calculator is something I’ve been wanting in my clinic for the last decade, so I’m personally excited to be able to use it,” says Dr. Tendulkar. “The ultimate goal for the personalized risk estimator is to allow clinicians to identify patients who may be at higher risk of recurrence so they can offer them more aggressive treatment. Likewise, we can avoid overtreatment of those who are unlikely to benefit.”
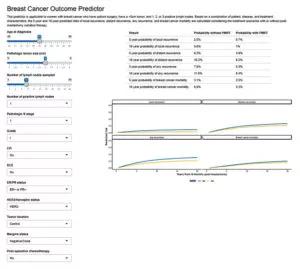
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6d0f509f-7bfb-4d91-9a23-4b0e8e2211b2/805x-Inset-Breast-Cancer-Outcome-Predictor-300x269_jpg)
As for future research, Drs. Sittenfeld and Tendulkar note that clinicians can look forward to data on the question of radiation or no radiation post-mastectomy from the nationwide randomized studies that are currently ongoing. They hope to use the database amassed for their model to study PMRT in other, more discrete subgroups, such as women who have undergone sentinel lymph node biopsy.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors