Cleveland Clinic performs its first balloon pulmonary angioplasties for the condition
Left untreated, chronic thromboembolic pulmonary hypertension (CTEPH) can lead to right heart failure and death. As detailed in this recent Consult QD post, pulmonary thromboendarterectomy is the gold-standard curative treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
However, surgery isn’t an option for up to 40 percent of patients with CTEPH, either because their clots are too distal to be accessible for surgical repair or because they have too many comorbidities to safely undergo surgery.
For those patients, Cleveland Clinic specialists are exploring a new option: balloon pulmonary angioplasty (BPA), a catheter-based procedure well established in its application for treating blocked vessels in the heart and brain.
Although use of balloon angioplasty in the lungs dates back 25 years, it was abandoned due to high rates of severe complications, including perforation and reperfusion edema.
Today, several centers in Japan have revived the procedure using modern equipment and techniques, with far better results.
In the fall of 2015, Cleveland Clinic pulmonologist Gustavo Heresi-Davila, MD, and interventional cardiologist Mehdi Shishehbor, DO, MPH, PhD, traveled to Japan for two weeks to learn the technique. And in early 2016 — with the help of Japanese specialists who came to Cleveland to assist — Dr. Shishehbor performed Cleveland Clinic’s first BPA procedures on two patients with CTEPH, both of whom were deemed inoperable due to distal disease.
Dr. Shishehbor treated each patient “without any complications and with immediate radiographic improvement in pulmonary blood flow,” says Dr. Heresi-Davila, Medical Director of the Pulmonary Thromboendarterectomy Program in Cleveland Clinic’s Department of Pulmonary and Critical Care Medicine.
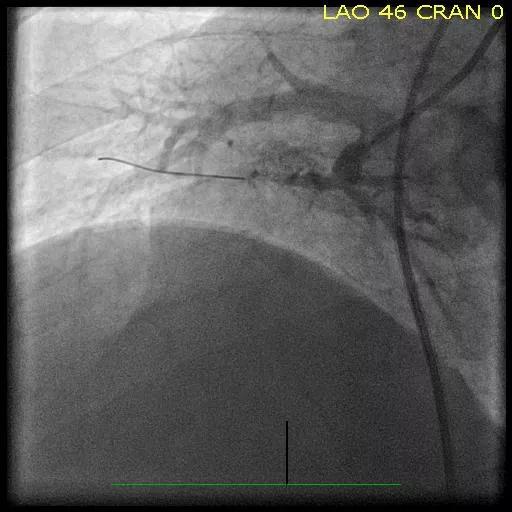
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d28c7573-6d95-46b1-84e0-b11b799a6e3a/Shish-CTEPH-Image-Inset-1_jpg)
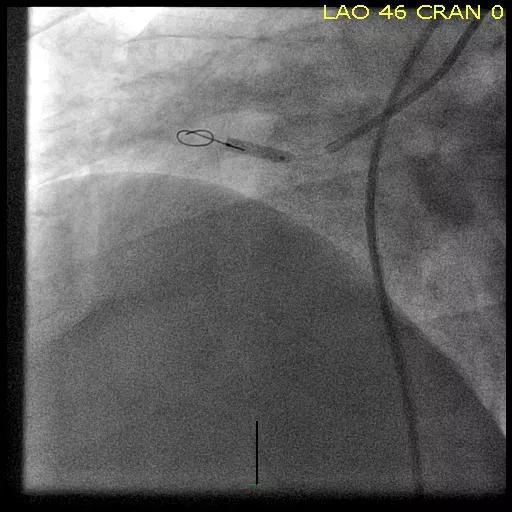
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/107127e6-62a1-48dd-af2d-931b840d11f1/Shish-CTEPH-Image-Inset-2_jpg)
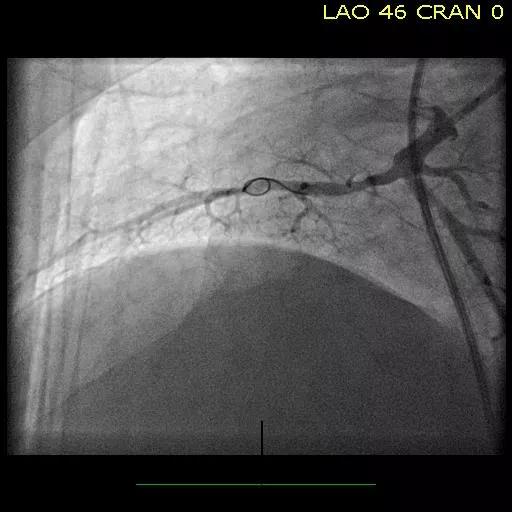
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8b91a2c8-37f6-47af-9ae3-51412217b383/Shish-CTEPH-Image-Inset-3_jpg)
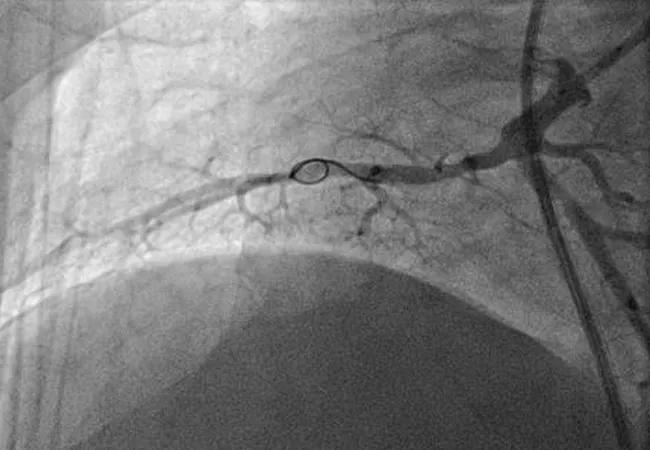
Figures. Imaging studies of the right lower lobe in one of the Cleveland Clinic CTEPH cases before (top), during (middle) and after (bottom) successful balloon pulmonary angioplasty.
Advertisement
Thus far, Cleveland Clinic is one of only three U.S. centers that have performed the procedure. “As we emerge as one of the premier CTEPH centers in the country, BPA is a welcome addition to the treatment armamentarium for patients with inoperable disease,” Dr. Heresi-Davila says.
Dr. Shishehbor, Director of Endovascular Services at Cleveland Clinic, foresees expansion of BPA here and at other specialized centers in the U.S. for the treatment of inoperable CTEPH, but he doesn’t see it replacing surgery for patients who can be treated surgically.
While BPA is far less invasive than thromboendarterectomy and patients are awake during the procedure, the arteries in the lung are very fragile and vulnerable to perforation. Moreover, to minimize the risk for reperfusion injury, BPA must be performed in two to five separate sessions — a process some patients might find difficult.
“Even if we get to the point of being very comfortable with angioplasty and can prove it’s safe and efficacious, I still think it won’t replace surgery,” Dr. Shishehbor explains. “I believe it will always be complementary.”
Nonetheless, the Japanese experience has been quite positive: Among approximately 700 BPA procedures conducted in about 170 patients over five years, there’s been zero mortality, a complication rate of less than 2 percent and only one case of restenosis. “They’re doing a very good job and have improved significantly over time,” Dr. Shishehbor observes.
Deciding whether a patient with CTEPH is a surgical candidate isn’t always straightforward, as it requires specific expertise — cardiothoracic surgeon, pulmonologist, interventionalist, cardiologist and others — in concert with patient and family input to determine whether the correct path is medical therapy, surgery, angioplasty or a combination.
Advertisement
“At Cleveland Clinic we take a global and multidisciplinary approach,” Dr. Shishehbor notes. “These patients are vetted very carefully.”
Another key to success, he says, is limiting procedures to a small number of surgeons, interventionalists and institutions in order to build expertise. For now, Dr. Shishehbor is the only person performing BPA at Cleveland Clinic, while a single surgeon performs the thromboendarterectomies.
“We are fortunate to have a high volume of patients, which allows us to do a lot of procedures and concentrate them so that surgeons become experts,” Dr. Shishehbor says. “We hope that by mastering these techniques in specialized centers of excellence, we can provide an alternative that supplements surgical options for these patients.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more