How we’re using a new multidisciplinary approach to broaden the benefits of ablation
Cleveland Clinic has adopted a novel multidisciplinary approach for improving the management of ventricular tachycardia (VT). The strategy involves management by a multidisciplinary heart care team to determine whether preemptive hemodynamic support can be provided to safely make VT ablation possible in patients who would otherwise be deemed too vulnerable to the procedure’s potential complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
VT occurs due to scar that develops following myocardial infarction or a slew of other possible etiologies, such as infection, inflammation and other types of nonischemic cardiomyopathy. Affected patients often require implantation of cardiac defibrillators for treatment of life-threatening VTs. While defibrillators are relatively effective, the electrical shocks they deliver can cause pain, psychological trauma and other harmful effects.
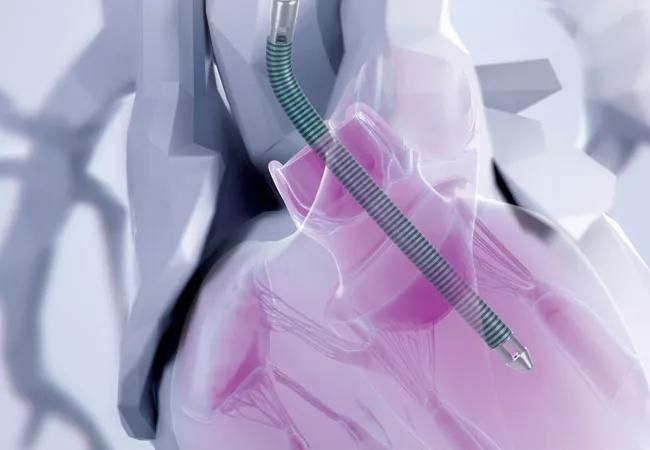
In response, VT ablation was developed as a percutaneous, catheter-based procedure that aims to eliminate sites critical for development of VT, thereby reducing the risk of recurrent VTs and defibrillator shocks. The procedure often requires induction of VT to allow accurate identification of those critical sites before they can be targeted with ablation. While VT can be induced safely in patients with milder heart failure and stable arrhythmias, induction is less safe in those with advanced heart failure and/or more complex arrhythmias. In these patients, induction of VT can lead to hemodynamic collapse and increased risk of complications, including death.
For years, a range of pumps have been used to provide temporary mechanical hemodynamic support to the failing heart during VT ablation, mitigating the risk of periprocedural acute hemodynamic failure. This practice has been limited, however, by insufficient circulatory support from the relatively small pumps that were available and their selective use in only the sickest patients. The past few years have seen development of larger and more effective pumps that can completely replace the function of the heart for periods of time. These pumps have been used at Cleveland Clinic for the past two years, including use to support VT ablation in critically ill patients, as detailed previously on Consult QD.
Advertisement
When electrophysiologist Elad Anter, MD, joined Cleveland Clinic in 2020 to lead its VT program, he recognized that about 90% of the institution’s patients with VT were referred or transferred after failed ablation attempts or because they were considered too sick to undergo ablation. He saw an opportunity to formalize a VT program comprising experts from multiple disciplines in addition to electrophysiology, including cardiac surgery, interventional cardiology, advanced heart failure and cardiovascular imaging.
Dr. Anter led the establishment of the multidisciplinary program, whose aim is to evaluate patients with VT and develop an optimal treatment plan for each patient. The plan may include changes to the medical regimen, ablation using a variety of hemodynamic support devices tailored to the individual’s heart conduction, and advanced heart failure therapies, including left-ventricular assist device implantation or heart transplant.
“VT usually occurs in patients with heart failure and should be addressed in the context of the overall heart condition and the patient’s well-being, plans and wishes,” explains Dr. Anter, Associate Section Head of Cardiac Electrophysiology.
As a leader in the development and application of mechanical support devices, Cleveland Clinic has embraced the full range of Impella and ventricular assist pumps to support patients in heart failure, undergoing VT ablation or undergoing high-risk coronary artery bypass grafting. Familiarity with the advantages of each model allows the heart team to customize device selection to each patient.
Advertisement
When a patient has mildly reduced heart function and relatively simple VT, the Impella CP® — a pump that is placed through a catheter in the groin and delivers about 4 liters of blood per minute — may be sufficient. In contrast, patients with more severe heart failure and/or complex arrhythmias require the larger Impella 5.0® or Impella 5.5®, which deliver more blood per minute. The size of the latter devices precludes catheter-based delivery and requires a minimally invasive incision in the shoulder. In some patients with right ventricular failure, a pump supporting the left ventricle may not be sufficient and an additional right ventricular support pump is needed.
In October 2019, the Impella 5.0 was replaced by the 5.5 version, which incorporated a key design change — removal of the curled “pigtail” tip of the device. “This made it easier to place surgically,” says Edward Soltesz, MD, MPH, Surgical Director of Cleveland Clinic’s Kaufman Center for Heart Failure Treatment and Recovery. “Without a pigtail irritating the ventricle, it is also less arrhythmogenic.”
Cleveland Clinic was the first U.S. center to implant the Impella 5.5 and is the top user of the Impella family of pumps in the U.S., having implanted more than 350 by the end of 2020. “Use of these pumps mitigates the risk of a disaster occurring during the ablation,” Dr. Soltesz notes.
In the electrophysiology lab, the electrophysiologist maps the heart to pinpoint the origin of the arrhythmia and ablates the location. Attempts to induce VT are made. If these attempts fail, the procedure is considered successful, and the patient is transferred to intensive care for observation.
Advertisement
After confirmation that the patient is stable and is maintaining good heart function, the Impella is removed. This may be done a few hours to two days after surgery. No anesthesia is required. If the patient has an implantable cardioverter defibrillator, it is left in place for backup.
Cleveland Clinic’s VT program provides a multidisciplinary platform for preemptively strategizing the treatment plan for each patient, including whether hemodynamic support is needed and which type is appropriate.
“Every patient referred for VT therapy is thoroughly evaluated by a team of electrophysiologists, interventional cardiologists, cardiac surgeons and cardiac intensivists to ensure that treating the arrhythmia is the right decision — and, if so, how it will be best accomplished,” says Dr. Anter. “Our new program facilitates collaboration among these specialists to provide effective and safe hemodynamic support during complex VT ablation procedures.”
“This preemptive approach is an excellent option, as it plays a major role in managing these critical patients,” notes Oussama Wazni, MD, Section Head of Cardiac Electrophysiology.
“This form of advanced life support enables VT ablation to be well planned and successfully accomplished by our heart team,” adds Samir Kapadia, MD, Chair of Cardiovascular Medicine and an interventional cardiologist on the VT ablation team.
“VT ablation is a high-risk procedure, due to the need to repeatedly induce VT to map the heart and identify the arrhythmogenic substrate,” Dr. Anter concludes. “As a result, many patients are told they are not candidates for it. However, this is the best solution for some patients with VT, and we need to make sure we can do it in the safest, most effective fashion possible.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more