The retrospective study identifies factors that influence disease-free and overall survival
Oral cavity and oropharyngeal cancers are aggressive malignancies that are difficult to treat and prone to recurrence. Worldwide, rates are increasing. Oncologists have had little up-to-date outcomes data to help guide treatment. “Most of the existing studies didn’t evaluate the factors that are associated with improved survival and functional outcomes. As newer alternative treatments to surgery, such as immunotherapy and other targeted agents, which allow meaningful long-term control of these recurrent cancers in some cases, it is crucial that we have more up-to-date data on outcomes of salvage surgery. If we don’t know how well patients do after salvage surgery, it’s difficult to counsel them on who should have the procedure,” says Brandon Prendes, MD, a surgeon at the Head & Neck Institute at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
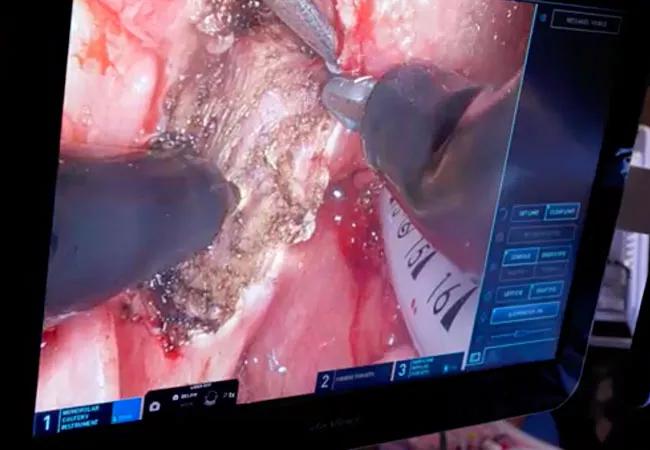
The Institute led a retrospective study of oral cavity and oropharyngeal cancer patients who underwent salvage surgery to investigate patient mortality and disease recurrence and which factors are associated with improved survival and functional outcomes. The findings appear in the October 2022 issue of Laryngoscope.
The study included 108 patients (72% oral cavity, 28% oropharynx) who underwent salvage surgery for recurrent oral cavity and oropharyngeal squamous cell carcinoma (SCC) from 1996 to 2018. They were followed for a median of 17.9 months; the median follow-up among disease-free survivors was 61.9 months.
The population was predominantly male (66%) with a median age of 62 years. Patients with oral cavity cancers tended to be older than those with oropharyngeal cancer. Most patients were current or former smokers (15.7% and 59.3% respectively). The initial tumor stages were: I/II (41.7%), III (12%) and IVa/IVb (46.3%). Oral cavity cancers had lower initial stage and grade and were less likely to be HPV positive. About a third of patients – 36% — had lymphovascular space invasion (LVSI).
Initial treatment for both types of cancer included: surgery only (25%), chemotherapy plus radiation (23.1%), radiation only (12%) and surgery plus chemotherapy or radiation alone (39.8%). Although oropharyngeal tumors were more likely to be treated initially with chemoradiation, salvage treatment was more likely to be surgery alone.
This study presents one of the largest published single-institution cohorts of outcomes for oral cavity and oropharyngeal salvage surgery to date and offers new insight into the factors that mediate these outcomes. It is the only study to report basic quality outcomes after surgery: Most patients (72%) had feeding tubes, half underwent free tissue transfer, a third required tracheostomy and a quarter were readmitted within 30 days of surgery.
Advertisement
Following salvage surgery, 52 patients experienced locoregional recurrence and 21 patients experienced distant metastasis. Disease-free survival (DFS) was less than one year (9.9 months) and overall survival (OS) was less than two years (21 months). Survival outcomes were not significantly different between oral cavity and oropharyngeal patients.
After oral cavity and oropharyngeal salvage surgery, adjuvant chemoradiotherapy, negative margins, negative LVSI and lower stage were associated with a lower risk of recurrence. Only lower-stage disease was associated with improved survival. LVSI and higher stage (III vs. I–II) were associated with worse DFS.
“This was the first study to identify LVSI as an important predictor of recurrence in a cohort of head and neck salvage surgery patients,”
“Overall, the findings drive home how serious these recurrent tumors are and reinforces how important it is to provide the best treatment at initial diagnosis. It’s a valuable update to the literature and will help guide future investigations.”
“The next step is to take these results and collect data prospectively on how well patients are functioning following treatment. Patients want to know about their chances of survival and their functional outcomes, such as swallowing and speaking, especially when they may have a limited lifespan,” says Dr. Prendes.
The Institute is currently conducting a study of cancer recurrence in a larger cohort of patients with larynx and sinus cancers. “As with oral cavity and oropharyngeal cancers, having accurate salvage surgery outcome data for this larger cohort will allow better comparisons to newer no-surgical treatment outcomes as they become more available.
Advertisement
“Considering how difficult oral and oropharyngeal cancers are to treat, prevention is really key. Not smoking and getting vaccinated for HPV, a major cause of throat cancer, could prevent these cancers from developing,” says Dr. Prendes.
A recent episode of the Head and Neck Innovations podcast featuring Dr. Prendes continues the discussion on this topic.
Advertisement
Advertisement

Case highlights the importance of oral hygiene in hospital and outpatient settings

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise