The approach and recent outcomes of the single-port transvesical simple prostatectomy
Surgical options for benign prostatic hyperplasia (BPH) have expanded significantly in recent decades—from the advent of laparoscopic and robotic simple prostatectomies in the early 2000s, followed more recently by single-site transvesical simple prostatectomy using the multiport robot.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The evolution of single-port robotic surgery has helped introduce yet another approach in the management of BPH. Urologists in the Glickman Urological & Kidney Institute at Cleveland Clinic have published two recent studies that describe and evaluate the performance of a new technique: single-port transvesical simple prostatectomy (SP TVSP).
In a recent multicenter study—the first of its kind—researchers evaluated perioperative and postoperative outcomes of the procedure in 91 patients. The team concluded that SP TVSP offers patients favorable perioperative outcomes, including low complication rates, generally shorter Foley catheter duration, and often same-day discharge. Functional outcomes were similar to those achieved through more traditional open and multiport approaches. The team published those findings in the Journal of Urology; the article was featured on the cover page of the journal.
These findings were reinforced in a separate single-institution study that evaluated outcomes from 42 consecutive patients undergoing SP TVSP. In the study, published in the Journal of Endourology, the authors report that all procedures were performed without complication, and 95% of patients did not require opioid analgesic after discharge.
Who is the ideal candidate for this approach? Jihad Kaouk, MD, Director of the Center of Advanced Robotic and Image-Guided Surgery at the Glickman Urological & Kidney Institute, says patients with urinary obstruction and a prostate size greater than 80 mL and for whom surgical management of BPH is recommended.
Advertisement
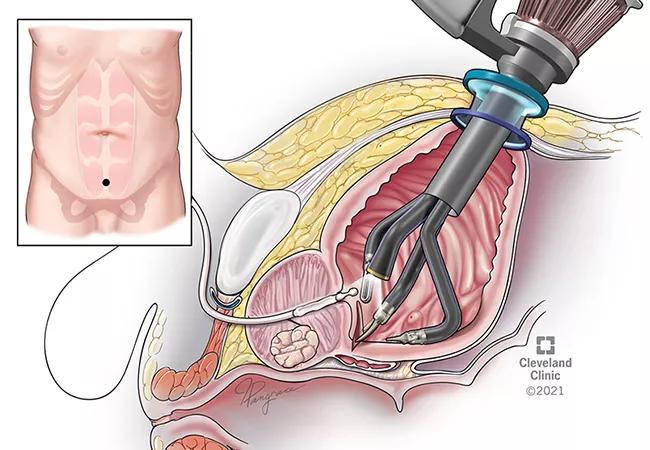
In the multicenter study, the surgeons at each center followed a similar surgical approach with some minor variations, the authors report. In all cases, patients were placed in the supine position, and the single-port robot was docked directly into the bladder through a single suprapubic incision to perform the prostatic enucleation.
Dr. Kaouk, senior author of the multicenter study, explains that the technique enables better visualization of the surgical field that is regionalized just to the prostate area. The use of the single-port robot means the surgeon makes only one small incision, surgical access through the bladder allows the surgeon to avoid the intraperitoneal cavity altogether.
“This has led to quicker recovery time. Patients generally stay at the hospital a few hours postoperatively, tend to report less pain, and we are seeing a decreased postoperative ileus because the bowel is untouched,” he says.
Study findings showed that the mean operative time across three centers was 159 minutes; the median postoperative hospital stay was 21 hours, with 42% of all patients discharged the same day; and the median Foley catheter duration was five days.
Importantly, at the nine-month follow-up, patients reported generally good functional and quality of life outcomes. Using the International Prostate Symptom Score (IPSS) with Quality of Life (QoL) system, a median of 4 and 0 were reported, respectively.
While there is some natural variability based on center protocols and surgeons’ preferences, the authors say these data were fairly consistent across the three centers.
Advertisement
These studies reinforce what Dr. Kaouk and colleagues previously reported. In 2020, they described this technique for the first time and published their initial experience in Urology. Good outcomes and no postoperative complications were observed in all 10 patients. They concluded that sparing the peritoneal cavity, minimum bladder dissection, and good visualization of the prostate were advantages of the SP TVSP approach.
The authors say functional outcomes appear to be similar to what has been documented with the multiport robot-assisted simple prostatectomy; however, improvements, such as reduced postoperative time with a Foley catheter, have been noted in the new technique.
They are hopeful that future studies, many of which are now underway, will offer a comparative analysis of the SP TVSP approach with the open and robotic simple prostatectomy in the treatment of BPH.
“These findings allow us to expand our study cohort beyond our institutional experience, get a deeper understanding of the SP TVSP approach in different institutional settings, and validate its utility,” says Dr. Kaouk.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key