Finding suggests need for multifront therapeutic approach
New research from Cleveland Clinic has identified for the first time a subtype of multiple sclerosis (MS) that lacks demyelinated lesions in brain white matter, casting new light on the long-established conception of MS as a disease characterized by demyelinated white matter lesions in the brain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The new subtype of MS, called myelocortical MS (MCMS), was found to feature loss of neurons and abnormalities on brain imaging that were indistinguishable from those of typical MS.
The findings, published online in Lancet Neurology by a Cleveland Clinic team led by Bruce Trapp, PhD, support the concept that neurodegeneration and demyelination can be independent events in MS. They also underscore the need for more-sensitive MRI techniques for evaluating brain pathology and monitoring treatment response in individuals with MS.
“This study is the first to provide pathological evidence that neuronal degeneration can occur independently of white matter demyelination in brains from patients with MS,” says Dr. Trapp, Chair of the Department of Neurosciences in Cleveland Clinic Lerner Research Institute. “To stop disability progression in MS, neuroprotective therapies may have to be used in combination with current anti-inflammatory therapies.”
Researchers have long investigated harmful processes that contribute to disease progression in MS. One such process is inflammatory demyelination, which occurs when the immune system attacks and breaks down the protective myelin that surrounds axons in the brain and spinal cord. Demyelination can cause neuronal degeneration, leading to irreversible disability in patients with MS. Many scientists believed that demyelination was the only reason why nerve cells in the cerebral cortex died in individuals with MS.
However, using tissue staining techniques, the Cleveland Clinic researchers observed that 12 of 100 postmortem brains obtained from patients with MS in their study did not exhibit cerebral white matter lesions indicative of demyelination. Using high-powered microscopy and MRI, they compared the brains and spinal cords from these 12 patients with MS (later characterized as MCMS) to the brains and spinal cords from 12 patients with typical MS and also to brains and spinal cords from individuals without any neurological disease. Although both the MCMS and typical MS groups had demyelination of the spinal cord and cerebral cortex, only the typical MS brains exhibited demyelination in the brain white matter (Figure).
Advertisement
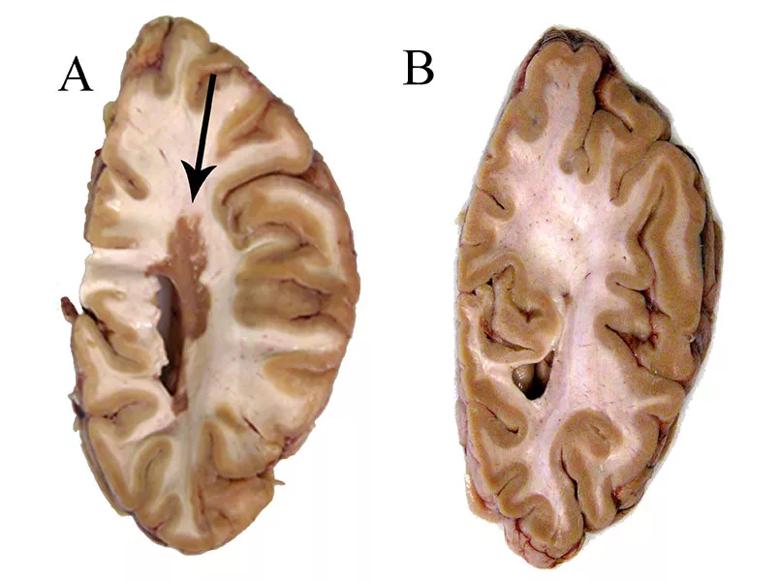
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/635edf0d-42c3-4c49-aa47-104f0b92eae1/18-NEU-4976-Trapp-Myelocortical-MS-inset_jpg)
Figure. Centimeter-thick slices from a typical multiple sclerosis (MS) brain (A) and a myelocortical MS brain (B). Whereas the typical MS brain contains a large white matter lesion (arrow), the myelocortical MS brain has no white matter lesions. Reprinted from Lancet Neurology (http://dx.doi.org/10.1016/S1474-4422(18)30245-X), Trapp et al., Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study, © 2018, with permission from Elsevier.
Despite having no cerebral white matter demyelination, the MCMS brains had reduced neuronal density and cortical thickness (two hallmarks of neuronal degeneration also observed in typical MS) compared with individuals without any neurological disease. Taken together, these observations show that cortical neuronal loss can, contrary to previous belief, happen independently of brain white matter demyelination in patients with MS.
Interestingly, however, clinical and radiological experts could not discern the difference between MRI scans of the MCMS and typical MS brains. Dr. Trapp explains that in MCMS, myelinated axons swell up. These swollen myelinated axons in MCMS MRI brain scans look highly similar to demyelinated axons in typical MS brain scans.
“The importance of this research is twofold,” says study co-author Daniel Ontaneda, MD, clinical director of the rapid autopsy program at Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “It suggests not only that we will likely need to attack MS and its causes from many angles, but also that we need to develop more-sensitive strategies for diagnosing and following the disease. Being able to correctly discern the swollen myelinated axons in MCMS from the cerebral white matter demyelination in typical MS will be critical for clinicians to explore tailored treatment strategies for patients living with MS.”
Advertisement
Additional research into the clinical differences between typical MS and MCMS will also be important, he adds.
The study was supported in part by grants from the National Institute of Neurological Disorders and Stroke (# P50NS38667 and # R35NS09730) and the National Multiple Sclerosis Society.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology