Study suggests limited role for CET in this cancer type
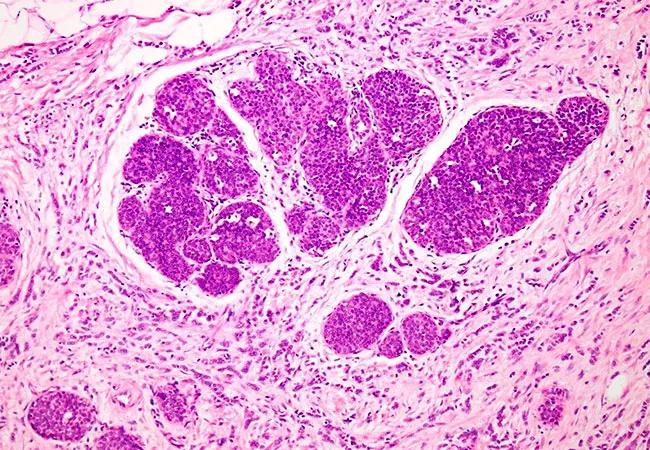
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5de41b00-7533-4134-a059-bb07e3922413/650x450-invasive-lobular-breast-cancer_jpg)
650×450-invasive-lobular-breast-cancer
The combination of adjuvant chemotherapy and endocrine therapy is no more effective than endocrine therapy alone in improving survival outcomes in patients with early-stage invasive lobular breast cancer, Cleveland Clinic investigators have found.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The research indicating a lack of survival advantage for the more rigorous chemo-endocrine therapy (CET) regimen over endocrine monotherapy (ET) in invasive lobular carcinoma (ILC) was presented at the 2019 San Antonio Breast Cancer Symposium.
The retrospective review also found that ILC patients treated at Cleveland Clinic did not routinely undergo testing with the Oncotype DX 21-gene assay to estimate the likelihood of cancer recurrence. But those who did usually were determined to be at low-to-intermediate risk, reaffirming the apparently limited benefit of CET in these cases.
“This is one of a few retrospective studies that specifically looked at lobular cancer outcomes and characterized these outcomes and Oncotype DX testing scores based on histology,” says Cleveland Clinic Cancer Center medical oncologist Megan Kruse, MD, the study’s principal author. “Our findings showed that the overall survival (OS) for lobular cancer patients was essentially equivalent, whether they received ET alone or CET. Disease characteristics such as tumor grade and patient age were prognostic but not predictive of the benefit of chemotherapy.”
Invasive lobular breast cancer accounts for approximately 10-15% of all invasive breast cancer cases and is the second most commonly diagnosed type of invasive breast cancer. Based on the insights from The Cancer Genome Atlas (TCGA) project, ILC has been established as a distinct subtype of invasive breast cancer only recently, in a 2015 publication. Despite its unique genomic and biological characteristics, however, ILC usually is treated with endocrine therapy, the same approach used for most other estrogen receptor-positive breast cancers.
Advertisement
“Only about 30% of women with hormone receptor-positive breast cancer are treated with chemotherapy, and this is usually driven by some type of genomic testing like Oncotype DX,” Dr. Kruse says. “For ILC, it is hard to estimate the proportion of patients treated with chemotherapy, but the data so far suggest that there is a fairly limited role for chemotherapy in this type of cancer.”
The study aimed to investigate whether ILC responds to CET and to uncover any potential associations between Oncotype DX results and response to CET.
Six hundred thirty-eight ILC patients with a mean age of 61.9 ± 11.7 years treated at Cleveland Clinic between 2004 and 2017 were included in the analysis. Four hundred six patients (63.6%) received ET alone; 232 (36.4%) received CET.
Dr. Kruse and her collaborators compared recurrence-free survival and OS between the two treatment groups, and analyzed any differences in outcomes between age and pathological propensity score-matched treatment groups. They also assessed the prognostic value of Oncotype DX testing in predicting cancer recurrence or patient death.
The investigators found recurrence-free survival (local or distant) to be worse in patients who received CET compared to those who received ET alone (81.9% vs 96.5% 5-year recurrence-free survival). When adjusted for age and clinical prognostic features, however, the risks of death and cancer recurrence were similar in both treatment groups.
“These findings are generally consistent with the findings of previous studies that indicate there does not seem to be a significant benefit of CET overall for this histology,” says Dr. Kruse.
Advertisement
She further explains that Oncotype DX testing is useful to identify patients whose cancer is likely to recur later in life, and those for whom chemotherapy can reduce the risk of recurrence. Of the 35% of patients in the study cohort who underwent Oncotype DX testing, most had recurrence scores in the low- (59%) or intermediate-risk range (39%). The researchers found no associations between the Oncotype DX score and cancer recurrence or patient death.
“Only about 30% of patients from our study who would have qualified for Oncotype DX testing actually had it done,” Dr. Kruse says. ”We do not know why that is, but I suspect it might be related to the preconceived notion that chemotherapy does not do much for lobular cancers.”
Dr. Kruse notes that the study findings reinforce the current treatment standards but also support an evaluation of how genomic assays are utilized in patients with ILC. “The patients who qualify for Oncotype DX testing should not have it omitted simply because they have lobular histology,” she says.
The current study results raise the question of whether chemotherapy confers a survival benefit in higher-risk patients. Additional research is needed to answer this, says Dr. Kruse.
“We have ongoing lobular cancer studies at Cleveland Clinic, both retrospective and prospective,” she says. “In a collaborative study with the Ohio State University Wexner Medical Center and the University of Pittsburgh Medical Center, we are looking at the overall outcomes of patients with ILC and comparing them with the outcomes of patients with invasive ductal carcinoma over the same period.”
Advertisement
Feature image: Photomicroscopy of invasive lobular breast cancer.
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality