Findings from ADHERE registry should help guide patient selection
Older age and lower body mass index (BMI) confer a higher likelihood of treatment success with upper airway stimulation (UAS) in patients with obstructive sleep apnea (OSA). So finds a large international multicenter registry study published in the European Respiratory Journal (2019;53:1801405). Women also fared better than men, but that association did not reach statistical significance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Findings from this study help us identify patients with OSA who are more likely to respond well to upper airway stimulation,” says Reena Mehra, MD, MS, Research Director of Cleveland Clinic’s Sleep Disorders Center and senior author of the article. “These findings set the stage for future studies to further elucidate age- and sex-specific differences in responsiveness to upper airway stimulation.”
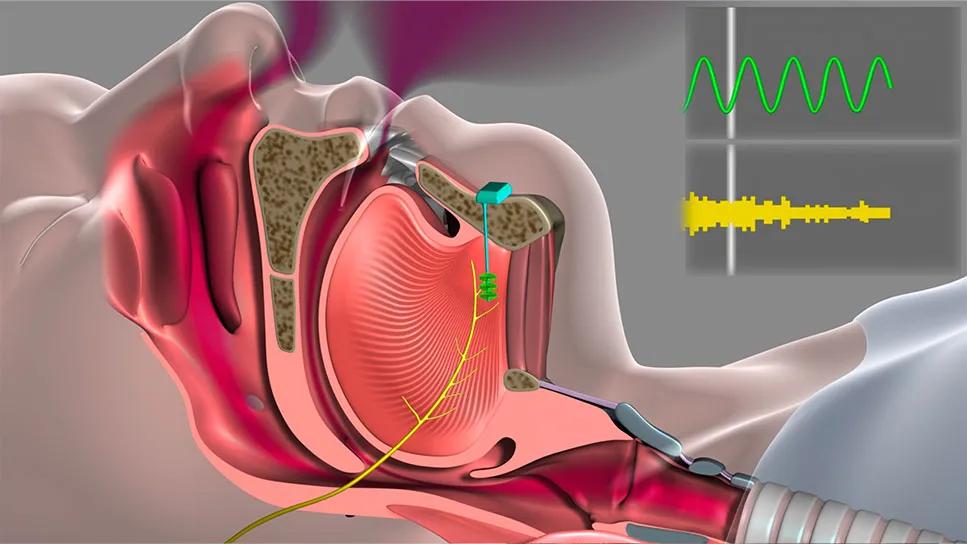
UAS, also called hypoglossal nerve stimulation, was approved by the FDA in 2014 for treatment of OSA, providing an important additional therapy option. Although OSA has been linked to multiple adverse health effects, it is often undertreated because many patients have difficulty tolerating continuous positive airway pressure (CPAP) therapy, the first-line treatment.
UAS involves surgical implantation of a cuff electrode that stimulates the hypoglossal nerve, prompting the tongue to move forward in the mouth and open the airway. A programmable neurostimulator and a pressure-sensing lead that detects respiration are also implanted (more details on UAS can be found in previous Consult QD posts here and here).
The new study analyzed data from October 2016 and January 2018 from the Adherence and Outcome of Upper Airway Stimulation for OSA International Registry (ADHERE registry), for which Sleep Disorders Center neurologist Tina Waters, MD, serves as principal investigator at Cleveland Clinic. The registry was established to systematically collect information on the use of UAS in clinical practice. It includes data on patient demographics, apnea-hypopnea index (AHI), Epworth Sleepiness Scale scores, objective adherence to UAS, adverse events and patient satisfaction from patients in the U.S. and Europe.
Advertisement
The study included 508 registry subjects enrolled from 14 centers in the U.S. and Germany. UAS was found to lead to substantial improvement of OSA, with median AHI reduced from 34 events per hour (denoting severe sleep apnea) to 7 (mild sleep apnea) and Epworth Sleepiness Scale measures from 12 (in excessive daytime sleepiness range) to 7 (in normal daytime sleepiness range) from baseline to the final visit at 12 months after implantation.
Patient satisfaction was found to be high, with patients rating UAS better than CPAP. The rate of adverse events was just 2 percent, with none meeting the study definition of serious.
In addition, the study found:
Dr. Mehra notes that while only 20 percent of registry enrollees were women, the study detected a trend of better treatment success in women relative to men. This association needs to be confirmed in a larger investigation, she adds.
Cleveland Clinic is one of several dozen centers worldwide that performs UAS at this time. The system is offered to selected patients with moderate to severe OSA and an intolerance to CPAP, according to Cleveland Clinic head and neck surgeon Alan Kominsky, MD, another co-author of the study.
Predicting success is especially important, as the therapy involves surgery as well as a high price tag. The device costs about $35,000 to place, with battery replacement costing additional thousands of dollars. Costs are frequently covered by medical insurance.
Advertisement
“The ADHERE registry now has data for more than 2,500 patients using UAS, representing a remarkable resource for investigations,” says Dr. Waters. “We look forward to more studies to help refine the use of this new device.”
Dr. Mehra notes that differences in response to therapy should guide further investigations of how UAS works at a basic physiologic level. She speculates that reduced collagen and elastin composition in ligaments or diminished tongue strength may occur with aging, leading to enhanced effects of nerve stimulation.
“Why are we seeing differences in response?” she asks. “Finding answers will help us drive this technology forward and allow us to develop personalized approaches to the treatment of obstructive sleep apnea.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help