A well-prepared team meets the distinctive needs of patients at hereditary high risk
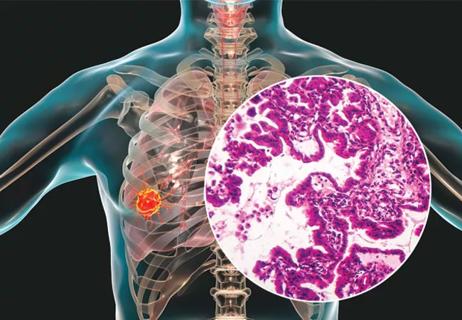
Patients with inherited risk for breast and ovarian cancer can benefit from a comprehensive approach that considers the complex medical and psychological needs associated with managing risk and making difficult decisions.
A multidisciplinary group of Cleveland Clinic specialists have developed such an approach in caring for patients with hereditary breast and ovarian cancer syndrome (HBOC), says Mariam M. AlHilli, MD, a gynecologic oncologist in the Ob/Gyn & Women’s Health Institute.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. AlHilli works with colleagues in the breast center, breast surgery, clinical breast psychology, plastic surgery, women’s health and genomic medicine in treating HBOC patients. The clinicians offer insights on delivery of complete care, including surveillance, medical and surgical preventive strategies, fertility, management of sexuality and menopause, and psychological support.
“Women with HBOC are commonly seen in clinical practice,” says Dr. AlHilli. “They can find themselves suddenly facing difficult medical decisions that may have profound implications for themselves and their families. A team of clinicians who understand these challenges can make a significant positive impact on the patient’s experience.”
Holly Pederson, MD, who introduced the hereditary high risk clinic in the Breast Center, agrees. “These families have been through a lot,” she says. “It takes courage to face and manage these risks. Having a team of providers who understand hereditary cancer can help.”
Early identification of women with red flags for HBOC is crucial so that they may be referred for genetic counseling, germline testing and preventive care. Trusted women’s healthcare providers, especially gynecologists, are well positioned to have important first conversations with their patients that yield relevant information.
“Young women often receive their primary care from their gynecologist,” Dr. Pederson says. “It is important that all women, but particularly Black women and those of Ashkenazi ancestry, have a formal risk assessment by the age of 30 such that early screening can begin.”
Advertisement
“We need to collect and assess the patient’s medical history as well as her family history,” adds Dr. AlHilli. “A personal or family history of breast cancer in those 50 and under, triple negative breast cancer, multiple primary cancers, male breast cancer, ovarian cancer, pancreatic cancer or metastatic prostate cancer should trigger a referral for genetic counseling.”
Those of Ashkenazi descent have a tenfold higher likelihood of carrying a BRCA mutation. Cleveland Clinic offers population testing to Jewish patients with or without family history, but certainly families of AJ descent with any of the above red flags should be strongly encouraged to pursue genetic counseling, the doctors say.
Surveillance for patients at higher risk for breast cancer typically may include mammography along with magnetic resonance imaging (MRI), beginning at different ages, depending on a number of factors, including which genetic variants are in play. Imaging includes:
Standard digital mammography. Two-dimensional screening imaging is now often reserved for pregnant women with highly penetrant mutations at the beginning of their second trimester. The minimal dose of radiation is safe, and screening should continue through pregnancy and lactation.
Digital breast tomosynthesis. Three-dimensional mammography improves detection of cancer and reduces false positives compared to 2D digital mammography.
Breast MRI. Offers improved detection of tumors, but it is associated with increased rates of false positives and increased cost.
Advertisement
Breast sonogram. Focused ultrasound is used if a suspicious area has been found on a mammogram or MRI, or if the patient has a breast symptom in need of evaluation.
The National Comprehensive Cancer Network website regularly updates screening guidelines. Ovarian cancer screenings generally are not sufficiently sensitive, so risk-reducing salpingo-oophorectomy remains the standard of care for managing patients at high risk, at an age appropriate for their individual risk.
Risk-reducing medications for breast cancer in patients carrying mutations in the BRCA1 and BRCA2 genes have been under-studied. Selective estrogen receptor modulators such as tamoxifen and raloxifene, as well as aromatase inhibitors (anastrozole and exemestane) reduce the risk of estrogen-receptor-positive breast cancer in other high-risk patients.
“Providers need to be comfortable in communicating the potential benefits (and risks) of these medications at appropriate life stages for high-risk women, and in considering medical co-morbidities and patient choice in the shared discussion,” says Dr. Pederson. “Generally, these medications are very underutilized.”
Combined hormonal contraceptives reduce the risk of ovarian and endometrial cancer in the general population and those with BRCA1 and BRCA2 pathogenic variants, and have been shown in multiple studies not to increase breast cancer risk.
Ultimately, however, patients at high risk are generally advised to undergo pelvic risk-reducing surgery, which includes bilateral salpingo-oophorectomy +/- hysterectomy. Those carrying variants for BRCA1 or BRCA2 who have the surgery have a 96% reduction in risk of developing ovarian cancer.
Advertisement
Clinicians treating patients at high risk for breast cancer, including those with pathogenic variants in BRCA1, BRCA2, PTEN, TP53, PALB2, STK11 and CDH1, should offer the patient a discussion around risk-reducing mastectomy (RRM), which is associated with a 90% to 95% reduction in the risk for developing breast cancer.
In addition to discussing the benefits of surgical options, caregivers and patients should thoroughly review the possible outcomes such as surgical morbidity, loss of satisfaction with body image, loss of breast sensitivity, and the small risk for developing breast cancer due to cells unavoidably being left behind. Mastectomy is an option and not a recommendation, as screening with MRI and 3D mammography is very sensitive in early detection.
“While overall, we see a great deal of patient satisfaction among those who choose RRM, it remains a very personal decision with a number of implications for the patient and her family,” says Dr. AlHilli. “It is important that patients understand that breast cancer risk cannot be totally eliminated by mastectomy, and that they will need to be followed annually.”
Pre-operative counseling with psychology providers who have experience in treating patients who have undergone risk-reducing surgeries can help support better outcomes by ensuring that all facets of the decision-making are considered.
Patients with hereditary cancer risks also may find themselves weighing decisions about family planning and assisted reproduction. Those who wish to preserve the possibility of childbearing, but perhaps aren’t ready, may consider egg or embryo freezing.
Advertisement
The choices that HBOC patients must make unavoidably involve a sense of loss. Psychological counseling can be an essential component for navigating fertility issues as well as myriad other challenges for those who inherit cancer risk: fear about developing cancer, the future, financial stressors, and informing relatives. Those with a history of anxiety or depression, as well as patients who are socially isolated or have an avoidant coping style, may require more intensive psychological support.
“Patients need psychological care that is part of a coordinated, consistent, team-based approach,” Dr. AlHilli says.
The symptoms and health consequences that accompany early surgical menopause and the resulting loss of estrogen may be associated with a decline in quality of life. Hormone therapy (HT) is recommended for patients with early surgical menopause (unless contraindicated) until around age 50 — the age of natural menopause.
In addition to protecting against related cardiovascular disease, osteoporosis, dementia and stroke, Dr. AlHilli says, HT can help maintain urogenital and sexual health. Two recent studies concluded that the use of HT does not affect breast cancer risk for BRCA mutation carriers. Women with post-surgical menopause who not take HT should be monitored for bone-density decline, treated for genitourinary symptoms of menopause, and counseled with regard to sexuality. Notably, the medical consequences of early surgical menopause must be considered, regardless of whether any individual is experiencing menopause symptoms.
Patients with inherited risks for breast and ovarian cancer need ongoing, multidisciplinary care for every stage of life. Special focus should be given to the effects of early menopause and the variety of psychological issues related to risk-mitigating surgeries, says Dr. AlHilli. A trusted team that provides consistent care and messaging can provide the patient a sense of confidence in her plans and choices, and the best chance for positive outcomes.
Advertisement

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Authors discuss ethical challenges associated with sponsored genetic testing
Universal testing could reduce expected costs compared to EGFR single gene testing

Research enables precision medicine beyond patients with changed mutational status

Program plays key role in diagnosis and management of genetic kidney diseases

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Genetic variants exist irrespective of family history or other contributing factors

CD36 loss-of-function variant accounts for large portion of risk in this population