Rare cancer presents as unresolved changes of the nipple
A patient arrives at your clinic with red scaling on the nipple or what looks like bleeding of the nipple. What do you do?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While it’s more common for these symptoms to be a sign of eczema or psoriasis of the nipple and areola, in rare instances, this could be a form of ductal carcinoma in situ (DCIS) that affects the cells of the milk ducts. Paget’s disease involves skin of the nipple, and is considered early-stage disease. However, in roughly 30-50% of cases, women who have Paget’s disease also have some type of underlying invasive cancer behind the nipple or deeper in the breast.
This condition can present solely as nipple changes such as a rash that does not improve and is sometimes mistaken for a skin condition like eczema, so it’s important to conduct a full workup if the area is not responding to topical treatments.
ConsultQD had the opportunity to talk with Cleveland Clinic Breast Surgery Specialist Stephanie Valente, DO, who sees patients with Paget’s disease of the breast.
Dr. Valente: It represents roughly 1-3% of all breast cancers. It usually occurs in women who are 60 and older, but can occur at any age. DCIS is a form of pre-invasive breast cancer (stage 0) where cancer cells are starting to form but have not spread or invaded outside of the milk ducts. Most times DCIS only involves the breast ducts inside the breast, not right at the nipple. Paget’s disease is the name given to DCIS that involves the nipple.
Dr. Valente: When a patient has nipple changes with no palpable lump, the first thing their doctor will usually try is a steroid or fungal cream. If it doesn’t fully clear up after two weeks, it’s prudent for their doctor to refer them to a breast specialist as well as to get a diagnostic mammogram.
Advertisement
Dr. Valente: We administer a local anesthetic and then perform a skin punch biopsy of the nipple in the office.
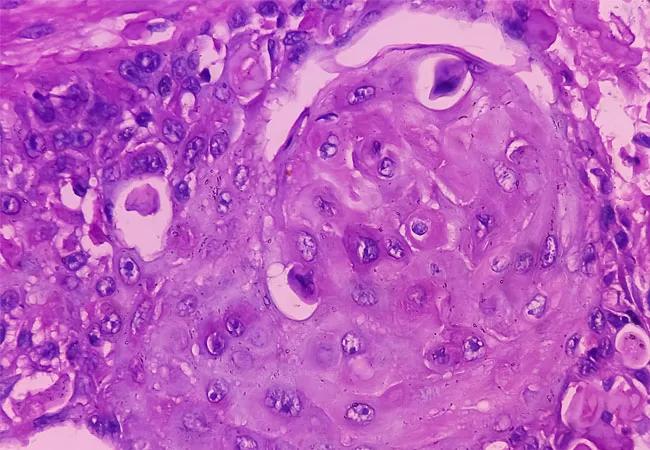
The pathologist can determine 100% from that if there is cancer in the nipple. The biopsy will either show skin changes consistent with dermatitis or a dermatology condition or Paget’s disease of the nipple, or sometime can diagnose an invasive cancer.
We also always make sure that the patient has an updated (diagnostic) mammogram and ultrasound to look behind the nipple, due to the high number of cases where there’s an underlying cancer. Most of the time if there’s disease in the nipple, that’s just the tip of the iceberg and there is underlying cancer within the breast.
Dr. Valente: Sometimes imaging would show a thickened skin or nipple, but usually Paget’s presents as visual nipple changes, so it can be seen, compared to most other breast cancer. A skin punch biopsy is the definitive way to diagnose Paget’s disease.
Dr. Valente: Yes, even if you see something on imaging behind the nipple, you still would want to biopsy the nipple to make sure that it’s Paget’s of the nipple and not eczema of the nipple, because you could have eczema of the nipple and still have cancer. You want to be sure to have a definitive biopsy before determining if there is a need to remove the nipple as part of the cancer operation.
Dr. Valente: No. Although women with a family history of breast cancer are at higher risk of developing breast cancer themselves, 85% of women who get breast cancer have no family history. That’s why it’s important for people to see their doctor if they experience any changes in their breast.
Advertisement
Dr. Valente: Breast cancer in men is extremely rare, but it does happen. It’s more common in men who have a family history of breast or ovarian cancer, because they’re at higher risk of carrying the BRCA2 gene.
Dr. Valente: We treat Paget’s disease just like any other area that develops DCIS. The tissue with the disease needs to be completely removed, with a normal rim of healthy surrounding tissue to ensure it is completely removed. For DCIS of the nipple, the nipple itself as well as any other affected tissue is removed.
Patients can have a central lumpectomy, which means the center of the breast is removed along with the nipple. Keeping the remainder of the healthy breast requires the patient to also get radiation to the breast. Many times, estrogen hormone blocking medication will be prescribed to help prevent the DCIS from re-occurring. DCIS alone does not require chemotherapy, so neither would pure Paget’s disease of the nipple,
Dr. Valente: If the cancer cells are contained to the nipple ducts, a lumpectomy followed by radiation would be recommended. Some women choose to have a mastectomy instead of a lumpectomy because in some cases it may prevent the need for radiation.
Chemotherapy would not be used in those instances. That would only be involved if there is underlying invasive cancer.
Dr. Valente: It is not any more painful than any other lumpectomy surgery. It looks more painful than it is. Cosmetically, to not have a nipple is the biggest difference.
Dr. Valente: Our plastic surgeons use tissue from elsewhere in the body to remake the nipple and areola to look quite similar to the other breast. There is also 3D tattooing that can be performed to replicate the skin pigment of the areola.
Advertisement
Advertisement

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Reconsidering axillary lymph node dissection as well as depth of surgical margins

Ultra-Hypofractionated Whole Breast Irradiation and Partial Breast Irradiation Reduce Many Toxicities

Best practices for reducing toxicities

Partnerships with local social service agencies key to program success

Ongoing clinical validation refine breast cancer risk substratification

Phase 3 trial found no survival differences between weekly or biweekly doxorubicin/cyclophosphamide or between weekly or biweekly paclitaxel

Findings strengthen evidence for risk-reducing procedures