Patient receives liver transplant and a new lease on life
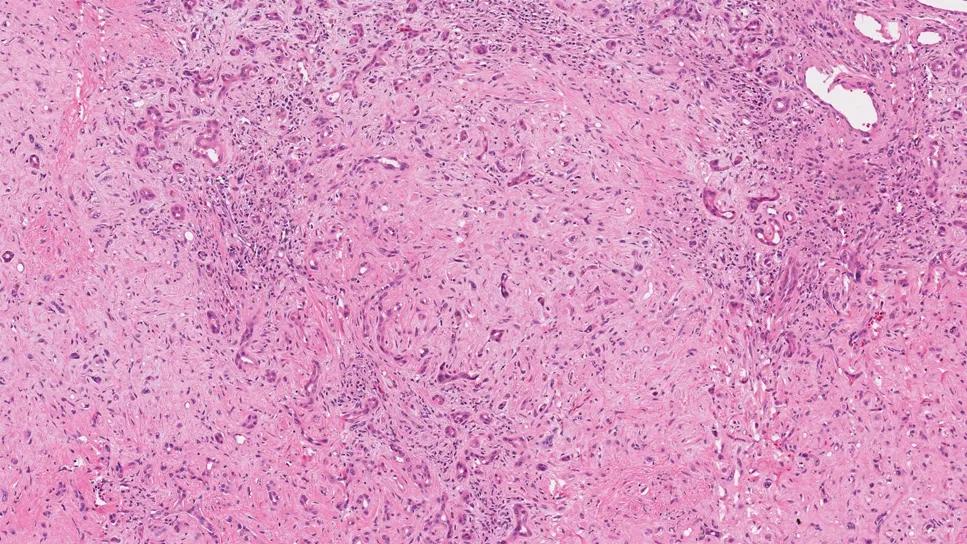
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b4cab17a-25e3-4d32-9336-63881be87b7a/ehe-pathology-patient-case)
Pathology image
A young man traveled from his home in South Carolina to Cleveland Clinic for a second opinion about his presumed diagnosis of stage 4 cholangiocarcinoma after developing end-stage liver failure from radioembolizations performed elsewhere. Upon reviewing his case, the Cleveland Clinic pathologist made a startling discovery: The patient did not have cholangiocarcinoma but in fact had a rare, indolent cancer called epithelioid hemangioendothelioma (EHE).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An otherwise active, healthy 45-year-old man was diagnosed at another cancer center with cholangiocarcinoma (bile duct cancer). He received four cycles of gemcitabine and cisplatin as well as two Y90 radioembolization procedures. The tumors did not respond to the treatment, and the radiation caused profound liver failure.
He reached out to Cleveland Clinic seeking a liver transplant after being told
elsewhere that he was not a candidate for the surgery. The patient, who lived in South Carolina, arrived at Cleveland ill and jaundiced. His abdomen was swollen with ascites. He needed a paracentesis nearly every week, draining about seven liters of fluid each time. His bilirubin level was 12.1 and his sodium level was dangerously low at 118.
Cleveland Clinic pathologist Clifton Fulmer, MD, PhD, reviewed the case, including the previous pathology from the outside hospital. While the morphologic features seen on the slides were unequivocally neoplastic, they were not classic for cholangiocarcinoma or any of its variants, and the imaging features didn’t fit the profile of the disease. In addition, the blood-based tumor marker for cholangiocarcinoma was only weakly elevated.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d238369a-8d8e-45ba-a2b1-2d7d49ac801e/ehe-pathology-patient-case-inset-1)
Following careful review, Dr. Fulmer was able to perform additional diagnostic testing on material from the previous biopsy. Based on these studies, he recognized that the patient had an EHE tumor, not cholangiocarcinoma.
"When performing second opinions, it's crucial to investigate the case more. If things don't seem to fit right, get more data,” says Cleveland Clinic oncologist Suneel Kamath, MD. “Do more diagnostic workup and really challenge what the underlying diagnosis is. In this situation, the pathology was an integral part of the case.”
“Second opinion and subspecialty consultations are a big part of our practice at Cleveland Clinic,” say Dr. Fulmer. “Most of the time the original diagnosis is the correct one. We still review every patient’s case with a fresh set of eyes. The depth and breadth of subspecialty expertise we have here sometimes leads to us finding things that were previously missed.”
The team’s radiologists also reviewed the patient’s previous scans. "You could tell there were masses, but they were very nonspecific. That was another tipoff that perhaps something else was going on,” says Dr. Kamath.
The liver surgeon, liver cancer specialist and hepatologist then came together for the initial consult to perform a comprehensive evaluation from day one. "With cases like this, expediency of getting appointments and coordinating care is essential. Having these three visits in one day helped get things rolling faster,” says Dr. Kamath.
There was a concern about small lung nodules that the patient had and if this might impede the transplant, but it wasn’t feasible to biopsy or remove a nodule surgically. The specialists and radiologists reviewed the imaging carefully. They came to a consensus that the nodules were not metastatic and that the patient was a candidate for a liver transplant.
Advertisement
Due to the severity of liver failure, the team needed to act swiftly to expedite surgery. Performing a transplant workup for someone who lives out of state added a layer of difficulty.
The transplant coordinator, Amy McFarlin, served as a key point person, lining up appointments over consecutive days when the patient could be in town. Working off a detailed checklist, they made sure all steps were taken to ensure the patient met transplant eligibility. “Being very systematic and methodical about these processes made all the difference,” recalls Dr. Kamath. “We were able to perform his transplant 2.5 months after the initial consult.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b1c0f234-0347-4008-9e01-1822113a294e/ehe-pathology-patient-case-inset-2)
In the weeks leading up to surgery, the team set out to help the patient be physically prepared for the transplant. They placed him on a regular schedule of diuretics to reduce fluid buildup and regular paracentesis procedures to help him to eat and maintain nutrition. The team also performed endoscopies to confirm that the patient didn't have varices.
In November 2022, the patient received his new liver. He tolerated the surgery quite well.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/73413ec3-7138-4113-bbca-de8ce919eb29/ehe-pathology-patient-case-inset-3)
As with a sizable fraction of patients, he experienced thrombosis in the hepatic artery shortly after transplant. This complication can result in ischemia of the organ. The team recognized the issue quickly based on liver function tests and an ultrasound, and successfully removed the clot and reconstructed the artery. By doing so, they were able to maintain perfusion of his organ.
Since EHE is a more indolent form of cancer and it had not metastasized, the patient did not need additional treatment. In the two and a half years since the transplant, he has had regular CT scans. The lung nodules proved to be benign, and there has been no recurrence of cancer.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d47b599f-3238-4de0-a658-c97154ff1221/ehe-pathology-patient-case-inset-4)
Incisive critical thinking is key in complex cases. Don't be afraid to get more biopsies or re-review the tissue and do your due diligence. “Have a high index of suspicion. That’s the way we catch these rare diseases,” says Dr. Kamath. “Don’t just accept the information you’re given. Think about the potential pitfalls of the data in the case. Was the right pathology diagnosis made? Does the imaging fit? Do labs fit? Does the treatment history fit with the story? If it does not, then collect more data about what's going on and involve other experts.”
It's not uncommon for people to be misdiagnosed with cholangiocarcinoma that actually is cancer that metastasized from colorectal or gastric cancer. “These tumors don’t look that different on a biopsy,” says Dr. Kamath. “You need a thoughtful and experienced pathologist in reviewing these cases.”
Having multidisciplinary teams builds trust. The Clinic’s liver cancer specialists, hepatologists and liver transplant surgeons regularly discuss cases together and collaborate closely with their radiologists and pathologists. Having confidence in the expertise of each team member was instrumental in reviewing the case and determining if the lung nodules would impact the patient’s ability to receive the transplant. “We had a lot of trust in one another’s judgment and in our radiologist who re-read the CT scan,” says Dr. Kamath.
Building relationships improves access to care. Cleveland Clinic has established itself as a preferred hospital for second opinions. “We have many relationships through our virtual second opinion program and through traditional insurance channels,” says Dr. Kamath. “That allows us to extend our care to more people nationally and even internationally.”
Advertisement
Advertisement
Enhanced visualization and dexterity enable safer, more precise procedures and lead to better patient outcomes
Minimally invasive approach, peri- and postoperative protocols reduce risk and recovery time for these rare, magnanimous two-time donors
New research shows dramatic reduction in waitlist times with new technology
Cleveland Clinic study shows positive outcomes for donors and recipients
Program's approach maximizes donor safety without compromising recipients' outcomes
Program expands as data continues to show improved outcomes
Atypical cells discovered after primary sclerosing cholangitis diagnosis
Research examines risk factors for mortality