Notable cohort findings include abnormal saccadic eye movements, use of second-line DMTs
A shift toward earlier use of second-line disease-modifying therapy and widespread prevalence of abnormal saccadic eye movements are among notable findings from the latest published report of demographic and clinical features of pediatric-onset multiple sclerosis (POMS).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Pediatric-onset MS is now being diagnosed in increasing numbers of children, yet its pathogenesis and optimal management regimens remain elusive,” says Cleveland Clinic pediatric neurologist Manikum Moodley, MD, senior author of the report, published in the January 2018 issue of Journal of Child Neurology. “To contribute greater insight into these questions, we undertook this study to describe the POMS population seen at Cleveland Clinic over a recent 13-year period in terms of clinical characteristics and outcomes of treatment as patients progressed into adulthood.”
Together with adult MS specialist Mary Rensel, MD, and other Cleveland Clinic colleagues, Dr. Moodley retrospectively identified all patients who presented to Cleveland Clinic and received a diagnosis of MS between 2002 and 2015 with a first attack occurring before age 18. Of the 64 patients who met initial criteria, four were excluded because of ongoing uncertainty of the MS diagnosis. For the 60 remaining patients, epidemiological, clinical, neuroimaging, laboratory and outcome data were collected and analyzed, as was detailed information on therapeutic management.
Mean age at presentation was 15.7 years, ranging from 2.5 years to 19 years. “The two-and-a-half-year-old patient represents one of the youngest POMS patients ever reported,” Dr. Moodley observes.
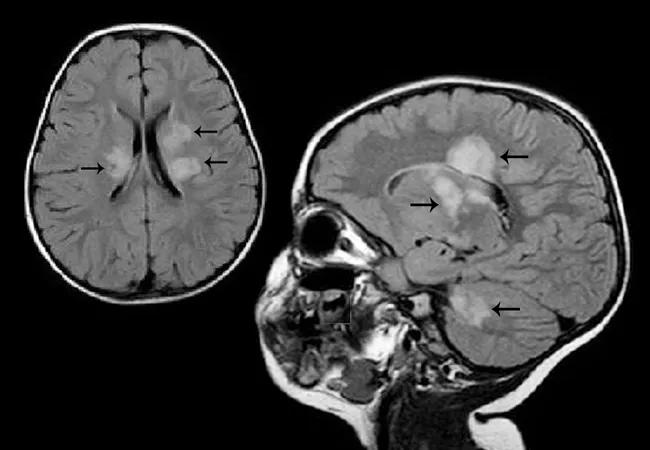
Many findings from this patient sample were consistent with prior reports of POMS, including general findings in terms of presenting symptoms, MRI findings and laboratory test results. Notable specific findings that confirmed previous literature reports of POMS included:
Advertisement
“These data lend support to proposed associations between MS and environmental triggers such as vitamin D deficiency and obesity,” notes Dr. Moodley.
A number of additional findings from this cohort differed from prior reports in notable ways:
“As anticipated, our study identified beta interferon as the most frequent choice of first DMT, followed by glatiramer acetate,” observes Dr. Moodley. While interferon continued to be effective for many patients throughout the follow-up period, he adds, other patients were resistant to interferon therapy. “A significant number of patients moved to stronger medications at early ages, requiring second-line DMTs currently approved only for use in adult MS.”
Advertisement
Use of three second-line DMTs was reported in the study: fingolimod, dimethyl fumarate and natalizumab. Of the 17 patients receiving one of these second-line DMTs at the end of follow-up, seven had started them before age 21, all without significant side effects.
The study authors identify use of these second-line DMTs in treatment-refractory patients as a priority for future POMS research. Trials of fingolimod, dimethyl fumarate and natalizumab in POMS are underway, Dr. Moodley says, noting that they will be critical for a more controlled assessment of these agents’ efficacy, adverse effects and optimal dosing in pediatric patients.
“Approximately 30 percent of patients with POMS will not respond to first-line therapies, hence the need for second-line agents,” he explains. “However, the International Pediatric MS Study Group urges pediatric and adult neurologists treating POMS to use extreme caution when considering second-line DMTs for pediatric patients because of side effects.”
An additional research priority spotlighted in the paper is evaluation for neurocognitive dysfunction. Despite a lack of formal assessment for it in this study, cognitive and/or memory dysfunction were identified by patients and their caregivers as prominent presenting symptoms, the researchers note.
“Our institution has adopted routine neuropsychometric testing for patients with POMS,” says Dr. Moodley, “but such testing was not always performed earlier in the study period, when understanding of cognitive impairment in POMS was still in its infancy. It’s now well known that brain growth and cognition are adversely affected in POMS. Future studies should focus on rigorous evaluation of testing measures to determine if there’s an association between early neuropsychological dysfunction and relapse trajectory.”
Advertisement
Dr. Moodley notes that additional emerging research questions in POMS include the role of remote infection with Epstein-Barr virus (EBV), low serum vitamin D levels, delayed infection with varicella zoster virus and exposure to maternal smoking. “There are ongoing studies looking at the impact of EBV on host immune function and also at vitamin D-related functions in patients with POMS,” he says.
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits