How it’s reducing length of stay, decreasing pain scores and limiting opioids
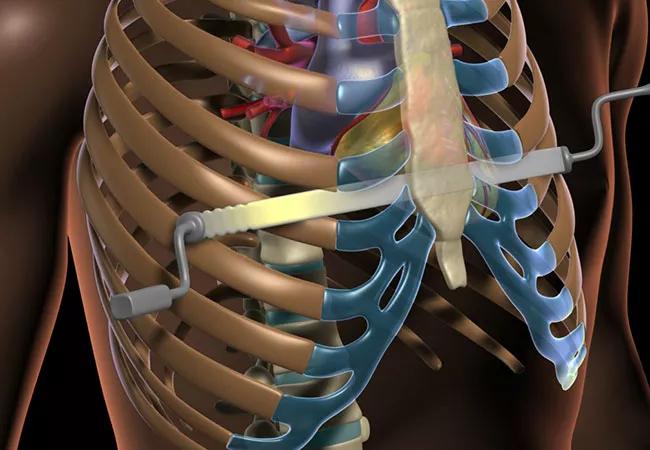
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b1c7e6d2-f1db-4df5-901a-2586cd231805/21-CHP-2394410-Hero-650x450-1_jpg)
21-CHP-2394410-Hero-650×450
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pectus excavatum affects approximately 1 in 1,000 live births and represents 90% of chest wall deformities. The Nuss procedure is the most common operation used to repair pectus excavatum and involves placement of a curved steel bar under the sternum to exert pressure anteriorly to correct the deformity. The entire procedure is done through two small axillary incisions 4 centimeters in length. The bar is removed three years later after sternal remodeling becomes permanent.
Patients typically undergo the surgery as teenagers, but the procedure is being performed in adults with increasing frequency. While it is minimally invasive, the process of placing a bar posterior to the sternum to elevate and remodel the chest is associated with significant postoperative pain.
Pain control remains the single most important factor contributing to hospital length of stay (LoS) following the Nuss procedure. Moreover, inadequate pain control can reduce patient satisfaction, limit mobility, increase opioid consumption, and increase healthcare visits and readmissions following discharge. For these reasons, optimization of postoperative pain is an integral part of caring for patients undergoing a Nuss procedure.
Historically, thoracic epidural was the mainstay of postoperative analgesia, but it was often limited by unreliable pain control, significant LoS and, in rare cases, substantial complications. Many groups, including our own, moved away from thoracic epidurals toward patient-controlled analgesia (PCA) after several studies, including randomized controlled trials, which showed no clear superiority between the two.
Advertisement
More recently, the addition of intercostal bupivacaine nerve blocks showed improvement in pain scores and LoS. Video-assisted intercostal nerve cryoablation (INC) is the newest method that surgeons are adding to their armamentarium during the Nuss procedure. Modern cryoprobes temporarily prevent pain transmission via rapid, localized freezing of nerves, which induces disruption of axons and demyelination (axonotmesis or a grade II nerve injury). This process leaves the fibrous neural structures including the epineurium, perineurium and endoneurium intact, and the process of Wallerian degeneration eventually results in axonal regeneration and reinnervation of the chest wall. Since nerve fibers can grow into their original endoneurial tubes, the original fiber pattern is maintained.
To assess the effectiveness of intercostal nerve cryoablation in the setting of our multimodality treatment protocol, we conducted a single-institution, prospective review of 40 consecutive patients undergoing the Nuss procedure for correction of pectus excavatum.1
Intraoperatively, intercostal nerves T3-T8 were treated bilaterally with cryoablation and intercostal bupivacaine nerve blocks. Exparel was used locally on the incisions. Our Enhanced Recovery After Surgery (ERAS) protocol included preoperative treatment with Gabapentin for four days, and with Celebrex and Tylenol for two days. These were continued in hospital and post-discharge. Oxycodone and valium were added immediately postop.
The vast majority of patients in this study (37/40, 93%) were discharged home the day after surgery, and 3/40 (7%) were discharged on postoperative day 2 for an average LOS of 1.1 days. The median average postoperative pain score was 2/10, and 8/40 patients (20%) took no oxycodone at all. Only 3/40 patients (7.5%) requested a refill of their 8-tablet prescription following discharge, and no patients were readmitted for pain control.
Advertisement
Our series remains among the largest published, and our outcomes are the most consistent for a series of that size. We have continued to accrue patients with the same outstanding results. We attribute our exceptional pain scores to the completeness of our pain control pathway, including our preoperative analgesic regimen (gabapentin, acetaminophen, and celecoxib), our use of intercostal bupivacaine nerve blocks (not used in other cryoablation studies) and cryoablation.
Pre-hospital analgesics and upfront use of both intercostal nerve bupivacaine injections and cryoablation prior to bar placement have the additional benefit of decreasing general anesthetic and opioid requirements intraoperatively. This may have helped in eliminating certain barriers to hospital discharge, such as nausea, somnolence and urinary retention, none of which were present in this series.
By three months postoperatively, 28% of the patients in our series had complete return of chest wall sensation. By six months postoperatively, 85% of our patients had completely normal chest wall sensation; and the 20 patients who have reached their 12-month follow-up, all report normal sensation. No patients experienced chronic neuropathic pain.
Before cryoablation-assisted pectus surgery, the month or more needed for recovery meant that school-age patients had to undergo surgery during summer to avoid missing classes. Now, the reduced length of hospital stay and recovery time gives patients greater flexibility in scheduling their pectus excavatum procedure. The positive results have made cryoablation a standard part of Cleveland Clinic’s pectus excavatum protocol.
Advertisement
In summary, intercostal nerve cryoablation combined with intercostal bupivacaine nerve blocks and a well-defined pre- and post-hospital ERAS analgesic protocol is successful in discharging patients one day after the Nuss procedure, eliminating the need for intravenous opioids and achieving excellent pain control. Return of nerve function took longer than expected, but 85% of patients who reached six- month follow-up and 100% of patients who reached 12-month follow-up had normal sensation with no areas of residual numbness. Importantly, there were no cases of chronic neuropathic pain.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/5DAZy_hS7Cw?feature=oembed)
Intercostal Cryoablation is Improving Pectus Excavatum Recovery
Listen: Dr. DiFiore discusses the cryoablation technique for pectus excavatum recovery in a Cleveland Clinic podcast.
Reference
About the author: Dr. DiFiore is Director of the Center of Excellence for Minimally Invasive Repair of Pectus Excavatum (Nuss procedure) and Surgical Director of the Fetal Care Center at Cleveland Clinic and Professor of Surgery, Cleveland Clinic Lerner College of Medicine at Case Western Reserve University.
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes