Some underlying medical and intraoperative conditions warrant caution

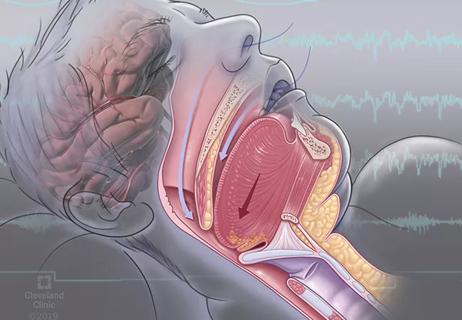
Respiratory failure occurs in as many as 3% of patients following surgery and is a major contributor to morbidity and mortality. New Cleveland Clinic research identifies risk factors for postoperative respiratory failure (PRF) in patients undergoing elective abdominal surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In addition to underlying medical conditions such as Type 2 diabetes and chronic obstructive pulmonary disease (COPD), the study reveals that several intraoperative factors are associated with higher rates of PRF. These include open surgery and increased net fluid amounts.
The findings can be used to identify higher-risk patients for additional monitoring or follow-up care, and to help inform surgeons and anesthesiologists in making the best decisions for their patients, says Cleveland Clinic Digestive Disease & Surgery Institute general surgeon Sofya Asfaw, MD, a coauthor of the study.
“This gives us insight on what factors can contribute to respiratory failure, which can significantly lead to morbidity and mortality in the postoperative period,” she says. While other studies have examined PRF risk factors generally, this is the first time researchers focused specifically on patients undergoing elective abdominal surgery, Dr. Asfaw notes.
Previous predictive models developed in an effort to reduce the incidence of PRF are based on the outcomes of patients who underwent multiple types of surgeries and are not specific to elective abdominal surgeries, meaning the risk factors in these particular cases are unknown.
For the retrospective case-control study, Dr. Asfaw and her colleagues reviewed the electronic medical records of 233 adult Cleveland Clinic patients who experienced PRF after undergoing elective abdominal surgery (excluding vascular, urologic and gynecologic procedures) between 2011 and 2016. Patients with respiratory failure or presence of tracheostomy at time of admission were excluded.
Advertisement
The researchers compared this cohort with a randomized, time-matched non-PRF control group of the same size.
They used Agency for Healthcare Research and Quality Patient Safety Indicator (PSI) 11 coding to identify patients with PRF. PSI 11 criteria for PRF are a secondary diagnosis code for respiratory failure; mechanical ventilation for 96 hours or more following the first major surgery; mechanical ventilation for less than 96 consecutive hours two or more days after the first major surgery; or a procedure code for reintubation occurring one or more days after the first major surgery.
Statistical analysis showed that PRF occurred in 1.2% of the 19,489 elective abdominal surgeries performed at Cleveland Clinic during the study period. Patients who experienced PRF were older than their non-PRF counterparts (63 years versus 52, p<0.001); had higher American Society of Anesthesiologists (ASA) scores (p<0.001); and more comorbidities such as chronic kidney disease, COPD, Type 2 diabetes, hypertension and hypoalbuminemia (p<0.05).
Surgeries resulting in PRF were more likely to be longer (4.13 hours versus 2.55 hours, p<0.001) and to involve laparotomy (77.7% versus 45.5%, p<0.001). Net intraoperative fluids were higher in patients who experienced PRF (3,635 ml versus 2,410 ml, p<0.001).
Patients who experienced PRF had longer postoperative hospital stays (20 days versus 5 days, p<0.001); higher reoperation rates (45.9% versus 3.0%, p<0.001); more complications (47.2% versus 14.2%, p<0.001) and higher mortality rates (19.3% versus 0.0%, p<0.001). Respiratory complications were the leading cause of death. Multivariate analysis confirmed the significance of age, ASA score, COPD, Type 2 diabetes, laparotomy and net intraoperative fluid balance as predictors of PRF.
Advertisement
Although surgeons cannot control their patients’ comorbidities, they could potentially reduce the risk of PRF by making changes in the operating room, Dr. Asfaw says.
She and her fellow researchers were surprised to find that the amount of fluids administered under anesthesia are a risk factor for PRF, although she says the finding makes sense.
It’s possible that excess fluid can contribute to intravascular swelling or congestion that could put additional stress on the lungs or other organs, Dr. Asfaw says. “Maybe we need to step back, take a pause, and ask, ‘Do we really need to be giving our patients all this fluid?’” she says. “This finding indicates judicious use of fluids is important.”
Another key finding: Laparoscopic or minimally invasive surgery is associated with a lower risk of respiratory failure than open surgery. A shorter operating time also reduced risk.
While the researchers did not evaluate the impact of types of anesthesia on PRF risk, they advise that regional anesthesia is preferable to general anesthesia and endotracheal intubation when possible, since the latter alters respiratory physiology and increases the likelihood of postoperative pulmonary complications.
Dr. Asfaw acknowledges that surgeons must consider many factors in deciding which type of surgery is right for their patient. “And in terms of operative time,” she adds, “we’d all like to be speedy in the operating room, but we want to be safe as well.” The risk of PRF should be one additional factor that surgeons take into account when making treatment decisions.
Advertisement
As a follow-up to the study, Dr. Asfaw and her colleagues will develop preoperative and postoperative guidelines and recommendations based on their findings.
In addition to takeaways for surgeons, Dr. Asfaw says the study yielded insights for hospital administrators and oversight bodies. The PSI codes are an important metric used by hospitals to monitor patient safety and track improvements, but the researchers found that the classification for respiratory failure was misleading.
PSI 11, the code for postoperative respiratory failure, defined PRF as any case where a patient remained intubated or had to be reintubated after surgery. However, this included patients with planned reintubations, such as patients who had a scheduled follow-up surgery two to three days after the initial procedure.
“Under the guidelines, that would qualify as a postoperative respiratory failure, even though truly, it’s not,” Dr. Asfaw says. “It has nothing to do with the patient’s ability to breathe on their own. I think we need to review and possibly update these definitions.”
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

Case study illustrates the potential of a dual-subspecialist approach

Findings show profound muscle loss variance between men and women

Treating a patient after a complicated hernia repair led to surgical complications and chronic pain
New tools and protocols to improve care

Endoscopic balloon dilation during pregnancy helps optimize outcomes
For the first time, risk is shown after accounting for underlying contributions of pulmonary disease

Surgery is typically the only option for the most severe cases, but a minimally invasive procedure is reducing morbidity and recovery time for patients