Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
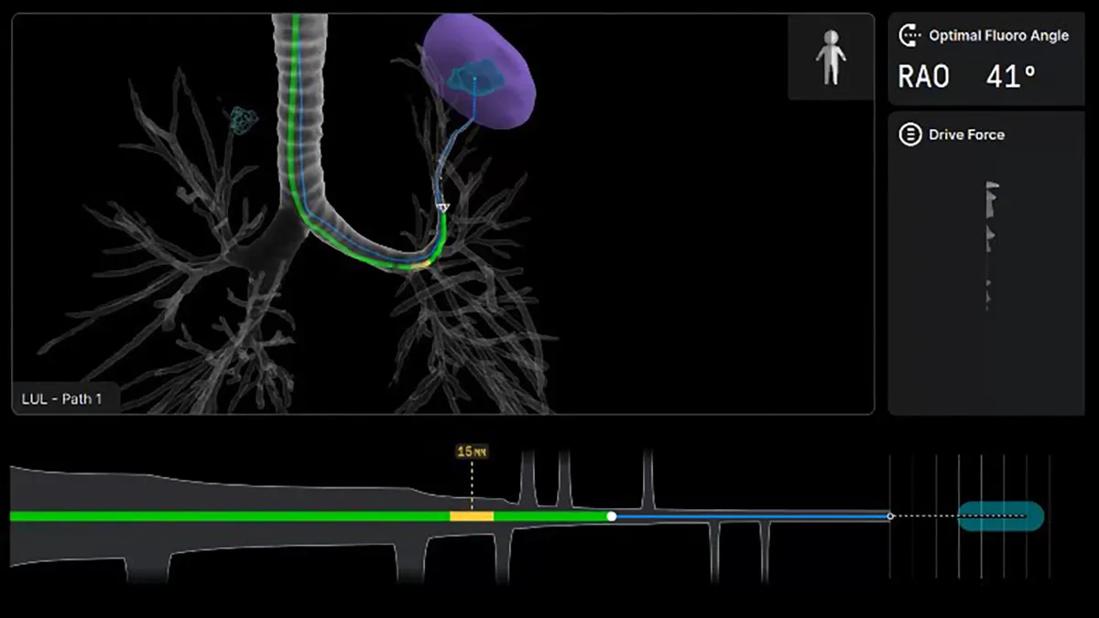
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/88fe8e3d-0252-4e07-8b54-33e8df384f18/Robotic-Assisted-Broncoscopy-screenshot)
Robotic-Assisted Broncoscopy screenshot
Navigational bronchoscopy technologies have transformed clinicians’ ability to biopsy hard-to-reach peripheral lung nodules. The latest evolution – robotic-assisted bronchoscopy (RAB) – is poised to surpass CT-guided transthoracic needle biopsy as the preferred approach for diagnosing early-stage lung cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As an early adopter of RAB, Cleveland Clinic Indian River Hospital performed its first case in 2022. Since then, the hospital’s Lung Nodule Clinic has leveraged RAB to enhance precision, safety, and diagnostic yield for patients with peripheral pulmonary nodules.
“Using robotic technology allows us to safely reach small, distal nodules with a very low risk of complication and achieve a highly accurate diagnosis, which ultimately leads to earlier treatment,” says Diego Maldonado, MD, FCCP, Section Chief of Pulmonary and Critical Care at Indian River Hospital.
Earlier this year, Indian River Hospital transitioned to a new robotic platform to align with Cleveland Clinic’s main campus in Ohio and sister sites in Florida. The Ion™ endoluminal robotic bronchoscopy system is one of three RAB platforms currently on the market that combines computer-assisted navigation with robotic catheter control.
“This platform change is an important step toward standardizing care, sharing data, and facilitating collaborative research across the Cleveland Clinic enterprise,” Dr. Maldonado explains. “Our sites will be aligned in diagnostic yield, complications, and other quality metrics, using the same standards and best practices.”
The coordinated use of a single system will also enable an enterprise-wide registry to advance RAB research – especially important given the absence of a national registry for robotic bronchoscopy outcomes.
The Ion system uses shape-sensing fiber optics embedded along the catheter to provide real-time, three-dimensional positional and orientation feedback. This, combined with advanced algorithmic guidance and a small 3.5 mm scope diameter, allows access to distal airways that were previously unreachable with conventional bronchoscopes.
Advertisement
Pre-procedural high-resolution CT imaging generates a virtual bronchial map that guides navigation to the target nodule, while intraoperative cone-beam CT or three-dimensional fluoroscopy confirms “tool-in-nodule” positioning during biopsy.
“The new system is exceptionally precise because of the scope size, catheter stability, and continuous 3D positional tracking,” notes Dr. Maldonado. “I can reach more distal nodules in the periphery with a high degree of accuracy.”
Cleveland Clinic’s three Florida sites and its main campus in Ohio will be among the first to receive newly approved software upgrades for the Ion system. These include AI-powered navigation that corrects CT-to-body divergence in real time and expanded imaging capabilities.
Historically, peripheral lung lesions were sampled via CT-guided transthoracic needle biopsy (TNB) performed by an interventional radiologist. Although TNB offers high diagnostic yield, pneumothorax rates are substantial.
“A number of studies have demonstrated that robotic-assisted bronchoscopy achieves diagnostic yields as high as 90% with fewer complications than transthoracic approaches,” Dr. Maldonado reports.
A recent multicenter randomized trial in The New England Journal of Medicine found that the diagnostic accuracy of navigational bronchoscopy (79%) was not inferior to TNB (73.6%), while the bronchoscopy group had a much lower pneumothorax rate – 3.3% compared to 28.3% in the TNB group.
Meanwhile, preliminary findings from the prospective, multicenter CONFIRM study, which evaluated the Ion system with integrated mobile cone-beam CT, showed tool-in-nodule success in 99.4% of cases and a strict diagnostic yield of 89%, with no pneumothoraces reported. The study included 155 patients with a median nodule size of 14 mm.
Advertisement
“The guidelines will likely change to reflect robotic-assisted bronchoscopy as the superior approach for diagnosing peripheral pulmonary nodules,” predicts Dr. Maldonado. “It’s a safer procedure, and I believe it will become the gold standard.”
The introduction of RAB at Indian River Hospital is already transforming lung cancer surveillance and management. In the pursuit of earlier diagnosis, when treatment is most effective, sub-centimeter nodules that were once monitored are now routinely biopsied.
“I can use robotic bronchoscopy to reach distal nodules as small as 0.5 centimeters,” Dr. Maldonado says.
Just five years ago, most of the lung cancers diagnosed by Dr. Maldonado were advanced stage. That trend is slowly shifting. “We’re turning things around with this technology – no question,” he adds.
Combining low-dose CT (LDCT) screening with molecular diagnostics such as proteomics and genomics enables much earlier detection in high-risk patients, especially smokers with small nodules. “If we have a patient with a 1-centimeter nodule who’s a heavy smoker with a strong family history of cancer, we don’t need to wait,” Dr. Maldonado explains.
Community education on LDCT screening remains a key priority. Current guidelines recommend screening for adults aged 50 or older with a 20 pack-year smoking history, who currently smoke or quit within the past 15 years.
“Unfortunately, too few eligible adults currently undergo annual screening – far below rates seen with other cancers,” Dr. Maldonado emphasizes. A recent national study found that only 18.4% of eligible individuals complete annual LDCT screening, underscoring the need for greater awareness and participation.
Advertisement
The Lung Nodule Clinic at Indian River Hospital manages patients with pulmonary nodules identified through screening or incidental imaging. Risk stratification determines who proceeds to robotic bronchoscopy.
If malignancy is detected, mediastinal staging with endobronchial ultrasound (EBUS) follows immediately. PET imaging and multidisciplinary review then guide the next steps in management.
“Our multidisciplinary team provides diagnosis, staging, and treatment planning in collaboration with thoracic surgery, radiation oncology, and medical oncology,” says Dr. Maldonado.
Looking ahead, Dr. Maldonado anticipates that RAB will continue to reshape lung cancer care. He points to ongoing studies exploring robotic-assisted bronchoscopy lung ablation using multiple energy modalities.
“Future advances in navigational accuracy and maneuverability will allow us to diagnose, stage, and treat localized disease during a single operative session,” he concludes.
Advertisement
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.
Cleveland Clinic Weston Hospital is actively recruiting patients for an international, multicenter, phase III study comparing MIS versus open interval cytoreduction following neoadjuvant chemotherapy in patients with stage IIIC-IV epithelial ovarian cancer.