Cleveland Clinic Weston Hospital is actively recruiting patients for an international, multicenter, phase III study comparing MIS versus open interval cytoreduction following neoadjuvant chemotherapy in patients with stage IIIC-IV epithelial ovarian cancer.
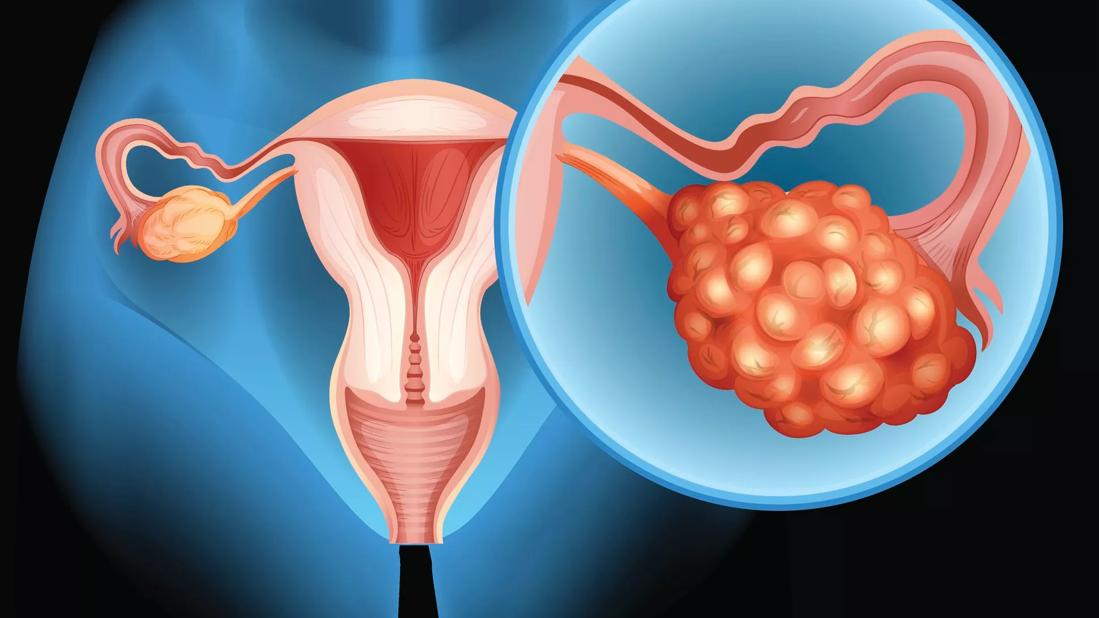
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8c4892b7-22d0-4adc-8453-a297ae9d483b/ovarian-cancer-GettyImages-486784816)
Ovarian Cancer
Ovarian cancer remains the most lethal gynecologic malignancy, responsible last year for more than 12,000 deaths and nearly 20,000 new diagnoses in the United States, according to American Cancer Society estimates. While incidence and mortality have declined modestly over the past two decades, the five-year survival for epithelial ovarian cancer (EOC) – the most common histology –remains stubbornly around 50%. For patients with metastatic disease, survival plummets to roughly 30%.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Unfortunately, about 75% of patients are diagnosed with stage III or IV disease, which carries a high recurrence risk,” states Joel Cardenas Goicoechea, MD, MBA, a board-certified gynecologic oncologist recently named Medical Director of Gynecologic Oncology at Cleveland Clinic in Florida. “We’re constantly reevaluating how to improve outcomes without compromising oncologic safety.”
One open question being explored is the most effective way to surgically remove all visible pelvic, abdominal, and retroperitoneal disease in cases of advanced ovarian cancer.
Traditionally, patients with advanced-stage ovarian cancer have undergone open cytoreductive surgery, a morbid operation that can involve a midline vertical incision from the xiphoid process to the symphysis pubis. “Our goal is to achieve maximal tumor debulking, a known prognostic factor in ovarian cancer survival,” says Dr. Cardenas.
However, with advances in surgical technology and chemotherapy regimens, the question of whether minimally invasive surgery (MIS) – laparoscopy or robotic surgery – can safely achieve the same oncologic endpoints has become increasingly relevant.
Over the past two decades, MIS has become standard of care in other cancers – notably endometrial cancer. Randomized controlled trials like GOG LAP2 and LACE demonstrated not only comparable survival outcomes, but also significant improvements in perioperative morbidity, pain, length of stay, and quality of life.
Yet, as Dr. Cardenas cautions, “We learned the hard way not to generalize these findings across all gynecologic cancers.”
Advertisement
The enthusiasm surrounding minimally invasive surgery met a sobering reality with early-stage cervical cancer. MIS for cervical cancer gained acceptance in the gynecologic oncology community before impact on survival and other cancer-related outcomes had been fully studied in randomized trials or large, observational studies.
Then in 2018 two pivotal studies published in the New England Journal of Medicine, including the LACC trial, revealed that minimally invasive radical hysterectomy was associated with worse overall survival and higher recurrence rates compared to open surgery. The following year the National Comprehensive Cancer Network(NCCN) issued revised guidelines recommending open abdominal radical hysterectomy for the treatment of early-stage cervical cancer.
“The entire field was in shock,” recalls Dr. Cardenas. “It was a clear lesson that we cannot extrapolate surgical strategies without evidence from properly designed trials.”
This philosophy underpins Dr. Cardenas' support for the Laparoscopic Cytoreduction After Neoadjuvant Chemotherapy (LANCE) trial, an international, multicenter, phase III study comparing MIS versus open interval cytoreduction following neoadjuvant chemotherapy in patients with stage IIIC-IV ovarian, primary peritoneal, or fallopian tube cancer.
Study participants receive three to four cycles of chemotherapy prior to undergoing either open surgery or MIS, followed by additional standard-of-care chemotherapy. Investigators will assess disease free survival as the primary endpoint, as well as overall survival, perioperative outcomes, and differences in health-related quality of life.
Advertisement
In the trial’s feasibility phase, which enrolled 100 women, complete gross resection was achieved in 88% of evaluable patients undergoing MIS (laparoscopic or robotic), compared to 83% in the open group. Based on these findings, the definitive phase is now underway to assess whether MIS can match or potentially improve oncologic outcomes.
Cleveland Clinic Weston Hospital is one of two enrollment sites in Florida and 19 internationally. The team’s first enrolled patient was randomized to open surgery, reports Dr. Cardenas. “I would encourage all eligible patients to consider enrollment. This is how we advance the field,” he adds.
While the use of MIS for early-stage ovarian cancer has increased in the United States, open surgery remains the standard of care. Current NCCN guidelines recommend that MIS be limited to carefully selected patients and performed by experienced surgeons.
“Our team in Weston has extensive experience performing open, laparoscopic and robotic-assisted surgery for ovarian cancer,” states Dr. Cardenas. “I’ve personally performed more than two dozen robotic-assisted cytoreductions and many laparoscopic cases.”
He emphasizes the importance of not rupturing ovarian masses during resection, especially in early-stage disease. “A rupture can upstage the cancer and change the treatment course, often requiring adjuvant chemotherapy.”
Dr. Cardenas also reports a growing number of patients – particularly those with a family history of ovarian cancer– seeking risk-reducing salpingo-oophorectomy following genetic testing. He notes that about 20% of ovarian cancers have a hereditary component, most commonly involving BRCA1 and BRCA2 mutations.
Advertisement
“I perform all prophylactic surgeries robotically,” he says. “Patients go home the same day, experience less pain, and recover faster.”
Dr. Cardenas credits his early experience with robotic technology for his proficiency with the approach. “I started doing robotic surgery in 2006, just after the FDA cleared the platform. The latest technology allows seven degrees of motion, 3D visualization, and fine dissection, which is particularly helpful in deep pelvic spaces.”
Dr. Cardenas underscores that ovarian cancer requires a multidisciplinary approach. In addition to a gynecologic oncologist, medical oncologist and radiation oncologist, patients may need the care of a liver, colorectal, and/or upper abdominal subspecialist. “At Cleveland Clinic Weston Hospital, we have that multidisciplinary capacity and are able to provide truly comprehensive care,” he states.
His team also performs HIPEC (hyperthermic intraperitoneal chemotherapy) for appropriate candidates– typically those receiving neoadjuvant chemotherapy followed by interval debulking.
With only 1,700 new ovarian cancer cases diagnosed each year in Florida, having access to high-volume, experienced centers is critical. Weston Hospital is a regional referral center for patients with ovarian cancer across all Cleveland Clinic locations in Florida.
Dr. Cardenas is optimistic but measured in his assessment of MIS in ovarian cancer. “Right now, most patients still require open surgery to achieve maximal cytoreduction. But for the select few, MIS may offer significant benefits, if we can prove equivalent oncologic outcomes.”
Advertisement
The priority is – and always will be – survival, he confirms.
For more information or to refer a patient for the LANCE trial at Cleveland Clinic in Florida, contact the Physician Referral Line at 833.733.3710.
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.