Genomic adjusted radiation dose guides treatment decision making
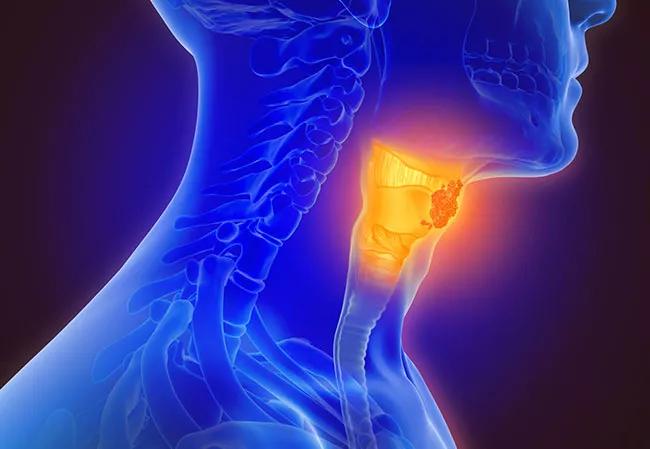
A recent study of patients with HPV-positive oropharyngeal squamous cell carcinoma (OPSCC) demonstrated that genomic adjusted radiation dose (GARD) predicts overall survival as a continuous variable, according to data presented during the American Society for Radiation Oncology (ASTRO) annual meeting. The findings also showed that GARD outperforms AJCC 8th edition (AJCC8) in prognostication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A multi-institutional team of researchers, including Jacob Scott, MD, DPhil, Associate Professor and Staff Physician-Scientist, CWRU School of Medicine and Cleveland Clinic, propose that GARD, which provides the first opportunity for genomic guided personalization of radiation dose, should be incorporated in the diagnostic workup of HPV-positive oropharyngeal squamous cell carcinoma patients and can be used to guide treatment decision making.
In a previously published pooled-analysis, Dr. Scott and colleagues showed that GARD is predictive of radiation treatment benefit and can be used to guide dose selection. In their current study, they explored the hypothesis that is possible to use GARD to predict overall survival in HPV-positive oropharyngeal squamous cell carcinoma patients who were treated with radiotherapy.
In this international, multi-institutional, prospective/retrospective observational study (NCT02832102), researchers analyzed gene expression profiles for 234 formalin-fixed paraffin-embedded samples from HPV-positive oropharyngeal squamous cell carcinoma patients. GARD was calculated for each patient.
A total of 203 patients received definitive treatment (chemoradiation or radiotherapy alone), and 31 patients underwent post-operative radiotherapy. The investigators used two radiotherapy dose fractionations for definitive cases: 70 Gy in 35 fractions or 69.96 Gy in 33 fractions. The median radiotherapy dose for definitive and post-operative cases was 70 Gy and 66 Gy, respectively.
Advertisement
Of the study participants, 29 received surgery and adjuvant chemoradiation, 14 underwent surgery and adjuvant radiotherapy and 19 were given radiotherapy alone. The median follow up was 46.2 months. Cox proportional hazards analyses were performed with GARD as a continuous variable and ROC analyses comparing the performance of GARD with AJCC8, according to the study authors.
Dr. Scott and colleagues reported that despite uniform radiation dose utilization, GARD showed significant heterogeneity, reflecting the underlying genomic differences in the cohort. Multivariate analysis revealed that each unit increase in GARD was correlated with an improvement in overall survival compared to AJCC8. “ROC analysis for GARD at 24 months yielded an AUC of 75.6 compared with an AUC of 73.9 for AJCC8,” they noted. “GARD ≥64.97 was associated with improved overall survival.”
“Understanding tumor radiation effects through GARD is superior to all other clinical factors and also dosing in order to understand outcome,” says Dr. Scott. “If you know the genomics, you can do a better job of treating patients.”
Based on their research, the study authors have derived a clinical nomogram that allows clinicians to use the genomic dose to more appropriately prescribe and choose radiation dosing.
“Right now, every patient with a given cancer gets the same dose of radiation, no matter who they are,” says Dr. Scott. “There are some differences based on indications. For instance, in head and neck cancer we know that HPV-positive cancers, in general, need less dosing than HPV-negative cancers. However, we don’t know from one patient to the next who will benefit from a reduced dose in the form of good cancer outcomes with less toxicity or who needs an increased dose in order to cure them. What this research really allows us to do is personalize that decision based on the individual patient’s tumor.”
Advertisement
Hear our podcast with Dr. Scott about predicting survival using GARD for HPV-positive oropharyngeal squamous cell carcinoma.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists