Study affirms XRT’s utility
Preoperative pelvic radiation (XRT), with or without concurrent chemotherapy, is safe and effective in patients with inflammatory bowel disease (IBD) and locally advanced rectal cancer, according to Cleveland Clinic research presented at the 2019 American Society for Radiation Oncology (ASTRO) annual meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
IBD is a risk factor for the development of rectal cancers, and IBD patients are frequently diagnosed with locally advanced cancers.
“Patients who have IBD are at a higher risk of developing rectal cancer compared to the general population, and also tend to have worse prognoses with locally-advanced cancers,” says Cleveland Clinic radiation oncologist Sudha Amarnath, MD, the study’s lead author.
XRT or chemo-XRT is the standard of care for stage II/III rectal cancer and is used to decrease the risk of local recurrence, explains Dr. Amarnath, but the utility of this treatment remains controversial in IBD patients due to toxicity concerns. Clinicians’ perception that pelvic radiation is too toxic for IBD patients is based on data published in the late 1990s.
The new study’s findings are important because they shed light on the degree of risk of short- and long-term toxicity from XRT, which is “the major reason that many radiation oncologists steer away from this treatment in patients with IBD,” says Dr. Amarnath.
“Because Cleveland Clinic is one of the largest IBD centers in the country, we see a number of patients with IBD and locally advanced cancers,” Dr. Amarnath says. By conducting this study, “we wanted to make sure that we are treating them to the highest standard of care … and that we’re looking back at our outcomes to see if this treatment is truly safe and efficacious in this patient population.”
“All of the study patients who went through treatment experienced mild or moderate toxicity that was well-managed – they did not require hospitalization or any extraordinary measures compared to the patients who are typically treated with preoperative radiation and do not have IBD,” says Dr. Amarnath. “There were no patients with grade 3 or above toxicity.”
Advertisement
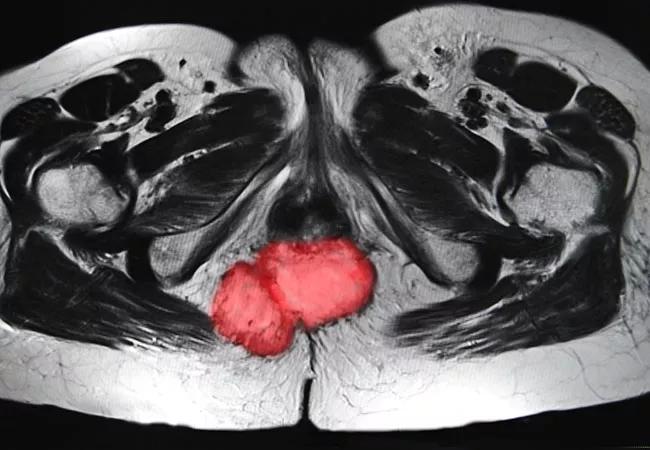
The retrospective study included 15 patients with IBD (nine with Crohn’s disease and six with ulcerative colitis) and AJCC stage II-IVA adenocarcinoma of the anorectum who underwent preoperative XRT (25 Gy/5fx) or chemo-XRT (capecitabine or CI-5FU and 50-50.4 Gy/25-28fx) between January 2014 and December 2018. The patients were followed for four to 33 months (median 17 months).
Twelve of the patients received concurrent chemo-XRT and three received short-course XRT. Five patients were on active IBD treatment during XRT. All patients completed treatment without breaks. Ten patients received intensity-modulated radiation therapy (IMRT)/volumetric modulated arc therapy (VMAT); the remaining five patients received 3D-conformal radiation therapy (CRT).
“The data from patient records was retrospectively reviewed to look at what doses they were treated with, what types of radiation treatment techniques were used, whether there was less toxicity with more modern radiation treatment planning, and to assess any patterns of recurrence,” Dr. Amarnath says.
None of the patients experienced acute (grade 3 or higher) toxicity. There were no differences in toxicity attributable to treatment technique. Grade 1-2 fatigue (73%) and grade 1-2 diarrhea (40%) were the most commonly reported treatment-related toxicities. Late toxicity was not observed in any of the patients at the last follow-up.
Fourteen of the 15 patients underwent surgery, six developed recurrences and four died of cancer in the follow-up period. A pathologic response to therapy was observed in most patients.
Advertisement
“This is the largest study to date of patients with rectal cancer and IBD and adds to a growing body of literature that seems to be showing that the toxicity profiles [in patients with IBD] are very much in line with those observed in patients who do not have IBD,” says Dr. Amarnath. “We are moving towards the recommendation that all patients with a locally advanced rectal cancer should be treated according to their stage of cancer and not the presence or absence of IBD.”
Dr. Amarnath says that one additional Cleveland Clinic study examining surgical outcomes of patients with IBD treated with and without pre-operative radiation is expected to be published this year. Moving forward, her team would like to investigate the role of XRT in patients with IBD and other types of pelvic cancers, especially gynecologic cancers.
“We need to continue to study and report on outcomes for our IBD patients so that all patients can receive the best possible treatment for their cancers,” she concludes.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient