Group sessions prior to prostatectomy may improve patient experience
A single one-hour preoperative group education session improved preparedness for prostatectomy among men with prostate cancer. And better preparedness, in turn, was linked to improved patient-reported urinary outcomes within the first year after surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those findings were reported at the 2019 annual meeting of the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction by Bradley C. Gill, MD, MS, study author and staff in the Glickman Urological & Kidney Institute’s Department of Urology.
Previous studies have examined the effects of both pre- and post-operative education sessions for men undergoing prostatectomy, demonstrating improved patient-reported outcomes.
“What hasn’t been shown before is exactly why. That’s why our question of preparedness came in. A lot of the side effects of prostatectomy deal with quality-of-life issues, which are entirely patient-reported,” Dr. Gill explains.
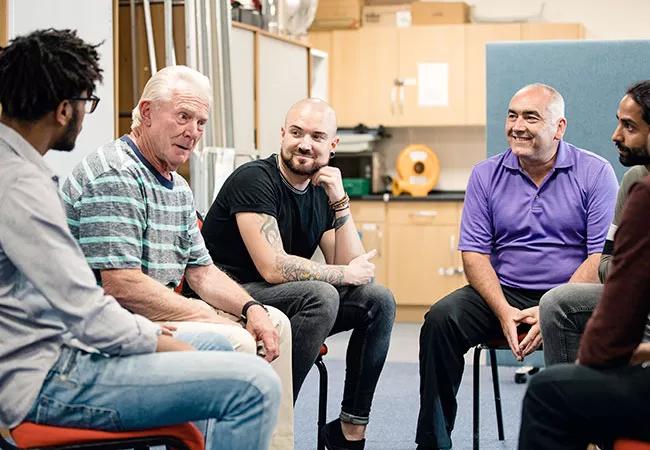
The group sessions were led by physician assistants or nurse practitioners with experience in caring for men undergoing prostatectomy. A total of 209 men with a mean age of 63 years at prostatectomy filled out baseline surveys prior to surgery and subsequent follow-up surveys at three weeks, as well as three, six, and 12 months post-surgery.
Visual analog scale (VIS) ratings demonstrated a high understanding of the side effects of the surgery (VIS score 80%) and what to expect in recovery (75%), including the fact that urinary leakage was a possibility (98%) and that recovery could take up to a year (94%).
Preparedness for recovery at home and overall feelings of preparedness were also high (78% and 82%, respectively).
Daily pad use (median [interquartile range]) decreased at the following assessment points: three weeks (2 [1-4]), three months (1 [0-2]), six months (1 [0-1]), and one year (0 [0-1]). At the same assessment points, most men reported their urinary control was good enough to complete their desired activities: 53%, 80%, 82%, and 79%, respectively. Overall, at those times, recovery of their urinary leakage was felt to be expected or better by 73%, 80%, 85%, and 81% of men, respectively.
Advertisement
Understanding that urinary recovery can take up to a year was associated with greater overall recovery satisfaction at three weeks (p<0.001) and at three months (p=0.035), but not thereafter.
Overall preparedness for surgery was associated with believing that their urinary control was good enough to complete their desired activities at both three months and one year (p = 0.019 at both time points).
These results dovetail with those for sexual function following prostatectomy that Dr. Gill presented this year at the annual meeting of the American Urological Association.
In written comments and phone interviews, some of the benefits of the class the men mentioned included having the chance to interact with other men and engage in helpful discussion on topics they hadn’t yet considered.
“Being in a group setting, asking questions, and hearing others’ questions reinforces that they aren’t going through this alone. Some also found it very helpful to bring a family member or friend with them,” Dr. Gill says.
The fact that the sessions were led by Cleveland Clinic providers who are involved in the patients’ care was also important.
“One of the big advantages patients report is being able to spend more time with their providers – not necessarily the surgeons, but the team members who are part of their care through the entire process,” he notes.
The team is now working to improve the classes and widen access to these preoperative sessions, starting with publication of the findings later this year.
Advertisement
The idea for the intervention came from one of the nurses who now is one of the class leaders.
“She thought a pre-operative class might be of interest. The big thing for us was the team approach. It’s the basis of what we do.”
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key