With a careful technique, surgeons can perform PN for tumors once deemed unresectable
With improvements and evolution in robotic technology, robotic partial nephrectomy (RPN) is proving more and more successful for larger, complicated tumors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jihad Kaouk, MD, Director, Center for Robotic and Image-Guided Surgery, Glickman Urological & Kidney Institute, and colleagues published a retrospective study in The Journal of Urology, in which they examined preoperative factors associated with conversion from partial to radical nephrectomy (RN).
“These are very complex cases that have been deemed poor candidates for RPN due to high tumor complexity, and they tend to be older and have poorer kidney function,” Dr. Kaouk notes. “If the entire kidney is removed, some of these patients will end up needing dialysis. So we are sparing them consequences that could hurt them as much or more than the cancer itself.
“We have been able to perform successful partial nephrectomies in 97 percent of patients who fit this profile at our institution,” Dr. Kaouk says, citing study results.
For this approach to be successful, three criteria must be met.
“First, the residual kidney must be viable,” Dr. Kaouk says, noting that postsurgery, a kidney remnant volume of less than 30 percent of original tissue volume may not be functional. An estimated glomerular filtration rate (eGFR) lower than 40 ml/min/1.73 m2 for bilateral kidneys and 20 ml/min/1.73 m2 for a solitary kidney will significantly increase the risk of postsurgery dialysis.
“Second, we must be able to resect the entire tumor and obtain negative margins,” he says. “In addition to completely resecting the cancer and preserving a viable kidney remnant, we must be able to achieve hemostasis and minimize the risk of postoperative bleeding.”
Advertisement
The study involved 1,023 RPN cases performed at Cleveland Clinic between 2010 and 2015. Researchers compared successfully completed and converted cases, assessing tumor characteristics and preoperative and oncological outcomes.
They found 3 percent, or 42 out of 1,023 cases, required conversion to RN. The most common reasons for conversion included failure to achieve negative margin on frozen sections, suspicion of advanced disease and failure of progress due to sticky and inflammatory fat or difficult anatomy. The conversion patients also had larger and more complex tumors.
The investigation’s conversion rate from RPN to RN was slightly higher than those reported in other published observational studies, which may be due to the fact that Cleveland Clinic attracts and treats patients with more complex tumors.
“We performed successful partial nephrectomies in 97 percent of these patients with complex kidney tumors,” Dr. Kaouk offers. “By extending indications for partial nephrectomy, we were able to avoid dialysis for some of these patients, and this is a very gratifying outcome.”
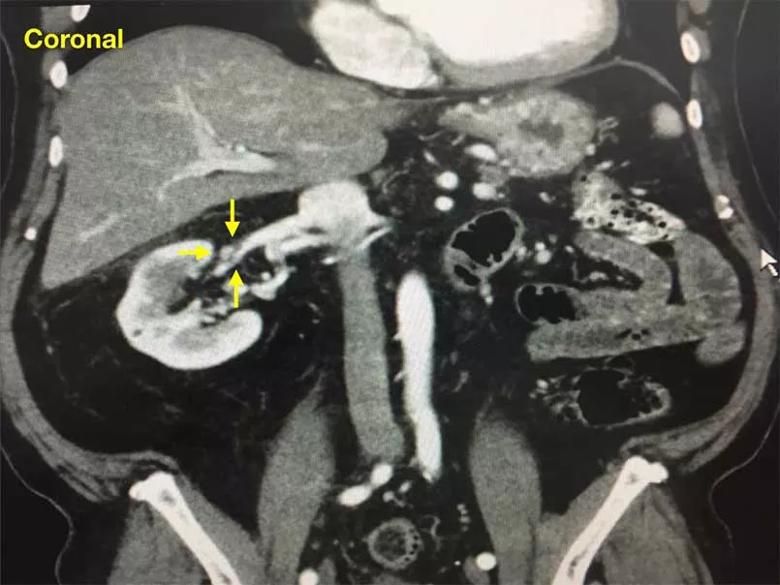
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4af675c3-436e-4976-a093-6a991216729b/805x-Robotic-Partial-Nephrectomy1_jpg)
Figure 1. CT scan of the abdomen (coronal) showing a 6.6 cm right renal mass on a solitary kidney with segmental renal vein thrombosis (arrow). R.E.N.A.L. score 10a.
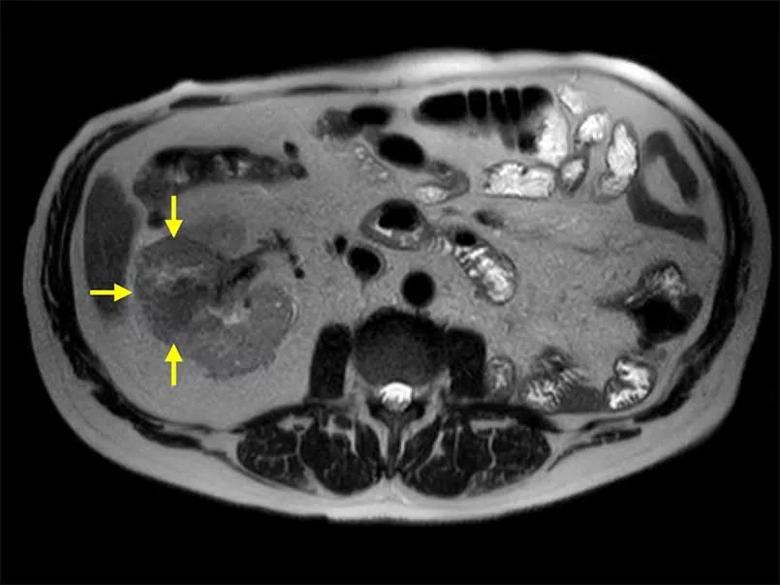
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2a104bcf-10c4-414a-ad49-e9a296dbc751/805x-Robotic-Partial-Nephrectomy2_jpg)
Figure 2. MRI of the abdomen (axial) showing a 6.6 cm right renal mass on a solitary kidney. R.E.N.A.L. score 10a
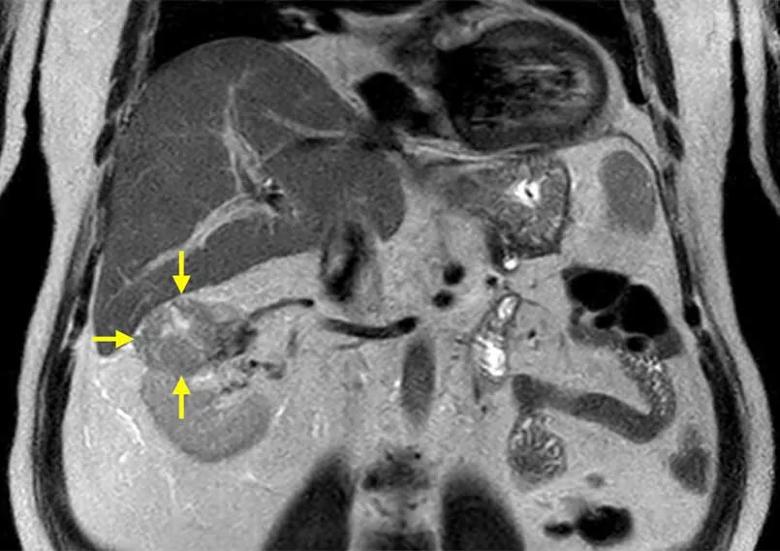
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/061527f4-5743-4eb0-b48d-346346426a49/805x-Robotic-Partial-Nephrectomy3_jpg)
Figure 3. MRI of the abdomen (coronal) showing a 6.6 cm highly complex right renal mass on a solitary kidney with a R.E.N.A.L. score of 10a.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key