Clinical trials testing olaparib in breast cancer
Update: The FDA approved olaparib for patients with BRCA-mutated, HER2-negative breast cancer in January 2018.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
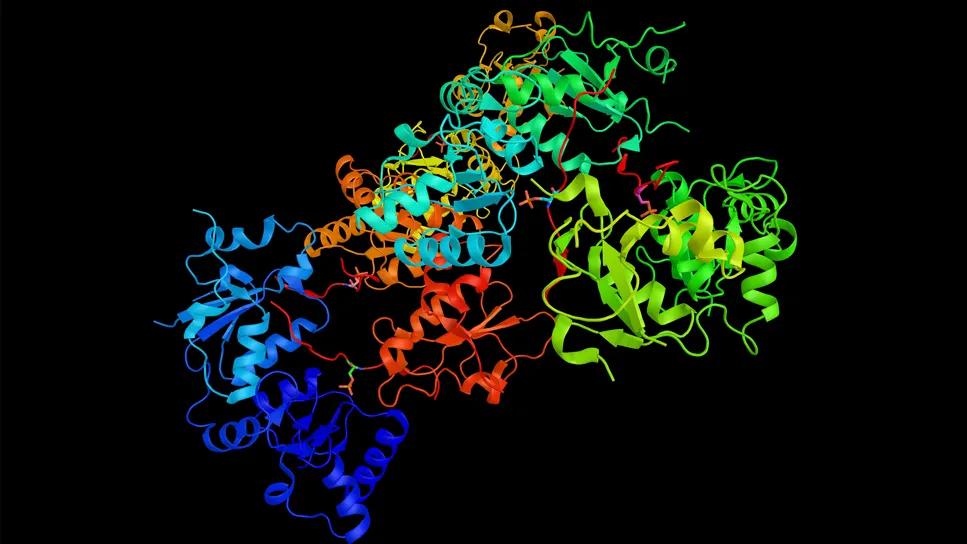
For patients with triple-negative breast cancer and BRCA1/BRCA2 mutations, current treatment options may at times be limited; currently, there are no specific treatments for BRCA1/BRCA2-mutated cancers that address the genetic defects seen in these cancers. However, there is growing interest in the use of Poly (ADP-ribose) polymerase (PARP) inhibitors in this setting.
“In patients with BRCA1/BRCA2 mutations, PARP inhibitors are one of the most promising treatments to be tested recently in clinical trials,” says Jame Abraham, MD, Director of Cleveland Clinic Cancer Center’s Medical Breast Oncology Program and Co-Director of the Comprehensive Breast Cancer Program.
PARP inhibitors interfere with base excision repair and therefore DNA repair, to effect death of tumor cells. PARP inhibitors can be highly lethal to tumor cells in patients who already have impaired DNA repair from BRCA mutation, Dr. Abraham says.
Although triple-negative breast cancer can be sporadic, these cancers share traits that involve DNA repair defects with those occurring in BRCA-mutated carriers. Eighty percent of hereditary BRCA-mutated cancers share the triple-negative breast cancer phenotype. The prevalence of BRCA1 and BRCA2 mutations in triple-negative breast cancer ranges from 4 to 14.3 percent, and an additional 27 to 37 percent have somatic inactivation of BRCA1.
As a class, PARP inhibitors can cause profound damage to cancer cells in breast cancers that involve DNA repair pathway defects. A number of PARP inhibitors are undergoing clinical development, but none is yet FDA-approved for breast cancer.
Advertisement
Cleveland Clinic is currently participating in two phase III clinical trials evaluating olaparib as a treatment for metastatic breast cancer as well as for stage II/III BRCA1/BRCA2, HER2-negative and triple-negative disease.
OlympiAD, the phase III trial on olaparib in metastatic breast cancer is ongoing but no longer recruiting participants and results are expected soon. In the meantime, Cleveland Clinic is enrolling patients in the OlympiA study, a phase III trial with olaparib as an adjuvant treatment for earlier-stage breast cancers with DNA repair defects — that is, in women with stage II and stage III breast cancer who have completed local treatment and neoadjuvant or adjuvant chemotherapy.
“We have enough evidence from metastatic breast cancer trials to know that olaparib is active in stage IV breast cancer. So now we want to see what kind of benefit stage II/III breast cancer patients will derive from use of olaparib,” Dr. Abraham says.
Olaparib was the first PARP inhibitor approved by both the FDA and the European Medicines Agency for patients with BRCA1/2 mutant ovarian cancer. In 2014, the FDA approved olaparib for patients with germline BRCA-mutated ovarian cancer who have undergone three or more lines of chemotherapy. The treatment was approved along with the BRACAnalysis CDx, a companion diagnostic test.
In the same year, the European Medicines Agency approved olaparib as maintenance treatment for patients with relapsed BRCA-mutated, high-grade serous ovarian cancer who have responded to platinum-based chemotherapy. In clinical studies, among the most common adverse reactions with olaparib were anemia, nausea, fatigue, vomiting, diarrhea, dysgeusia, dyspepsia and headache. In addition, myelodysplastic syndrome and acute myeloid leukemia have occurred in patients exposed to olaparib.
Advertisement
The new phase III trial on olaparib is enrolling patients with stage II and stage III breast cancer who underwent initial surgery and adjuvant chemotherapy. To be included, patients in this trial must either have triple-negative breast cancer (ER and PgR negative and HER2 negative; not eligible for anti-HER2 therapy) or ER and/or PgR positive, HER2 negative.
The randomized, double-blind, parallel group, placebo-controlled, multicenter phase III study will test a dose of 300 mg of olaparib administered twice daily for 12 months, while the control group will receive a matching placebo. The primary outcome is invasive disease-free survival, up to 10 years. Assessments will also include overall survival; distant disease-free survival; and the incidence of new primary contralateral breast cancers, new primary ovarian cancers, new primary fallopian cancers and new primary peritoneal cancers. Secondary outcomes also include patient-reported outcomes using the FACIT-Fatigue and EORTC QLQ-C30 Quality of Life questionnaires.
At baseline, gene sequencing will be used to identify patients who have BRCA mutations. During the trial, patient exposure to olaparib (in plasma) will be monitored in those women receiving the medication as adjuvant therapy. Safety and tolerability of olaparib will also be assessed in the trial.
“This newest phase III clinical trial on olaparib in women with stage II/stage III breast cancer will give us an idea of the efficacy of olaparib in earlier-stage cancers,” Dr. Abraham says. “This is a very good trial for investigating a potentially promising adjuvant therapy for women with BRCA1/BRCA2 and HER2-negative breast cancer in the earlier stages of their disease.”
Advertisement
He notes that no PARP inhibitor is yet FDA-approved for breast cancer and that other PARP inhibitors — veliparib and niraparib — are also going through clinical trials right now. (Update: The FDA approved olaparib for patients with BRCA-mutated, HER2-negative breast cancer in January 2018.)
Photo Credit: ©Russell Lee
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient