How to diagnose and treat
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The symptoms are nonspecific, and the treatment is often described to patients as worse than the disease. These are the realities facing patients with nontuberculous mycobacterial (NTM) pulmonary disease and the physicians who treat them.
Unfortunately, NTM pulmonary disease is underrecognized, underdiagnosed and undertreated. When a patient does receive a diagnosis, it is usually years after the onset of their symptoms. Diagnosis is challenging as symptoms tend to be attributed to underlying asthma or chronic obstructive pulmonary disease (COPD) or symptoms are those not traditionally associated with lung disease, such as fatigue, low appetite, weight loss, anxiety and night sweats.
Patients with bronchiectasis are particularly susceptible to NTM infections because their airways have lost the ability to adequately clear secretions and the microorganisms found within the lungs. Testing for and treating NTM infections in this population is particularly important because the earlier disease is recognized, the more likely treatment will result in a cure. Also, earlier treatment can slow the irreversible progression of bronchiectasis that chronic inflammation and infection are known to cause.
At Cleveland Clinic, we have a multidisciplinary approach that relies on frequent sputum cultures to develop tailored antibiotic regimens, respiratory therapy education to optimize aggressive airway clearance regimens, and adherence to the most up-to-date guidelines on the treatment of NTM pulmonary diseases.
Advertisement
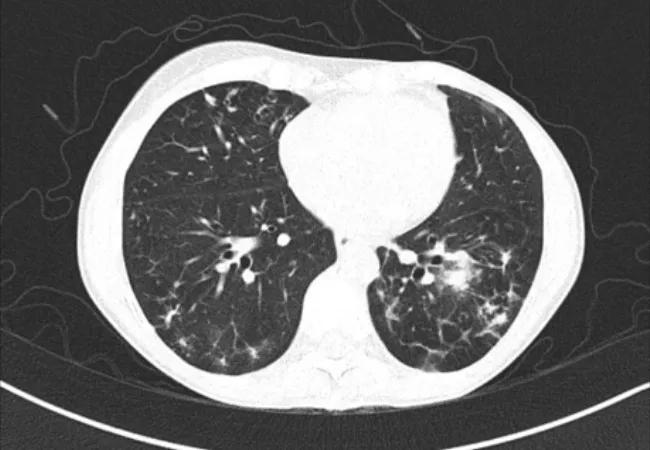
Pulmonary NTM infections due to organisms such as Mycobacterium avium complex (MAC) and Mycobacterium abscessus are being diagnosed with increasing frequency. These organisms are commonly recovered on expectorated sputum cultures or bronchoscopic cultures obtained as part of an evaluation for an abnormal CT chest demonstrating multiple pulmonary nodules or bronchiectasis.
The diagnosis of NTM infection is often less than straightforward, and decisions regarding treatment of NTM infections can be complicated. Some patients have underlying chronic lung disease that may need to be addressed first. Often, their underlying lung disease is blamed for their symptoms, and NTM is disregarded. This approach is not ideal as NTM infection can cause flares of underlying lung disease, thus treatment will lead to better control of their known chronic pulmonary conditions.
New guidelines published in 2020 emphasize the benefits of treatment earlier in most patients who meet criteria for lung disease as well as intensifying therapy if sputum cultures are still growing NTM despite six months of therapy. In the past, physicians steered patients away from treatment because the antibiotic regimens were felt to cause more burdensome symptoms than the NTM infection, but research has shown that earlier treatment allows patients to have a higher chance of cure and that antibiotic regimens are adequately tolerated in most.
When I lecture on what I wish I had learned in training, I discuss the importance of recognizing and prevalence of NTM infections. A combination of nonspecific symptoms and a low index of clinical suspicion contributes to a significant delay in diagnosis for these patients. More than half have suffered one or two years, often much longer, before the diagnosis is made and treatment begins.
Advertisement
As clinicians, we must raise our awareness of these infections. When a patient presents with fatigue and low appetite, a slow-growing lung infection isn’t usually on the radar. A patient with chronic cough and a clear X-ray oftentimes is suspicious for an indolent lung infection. If the cough does not respond to initial management, a CT chest is often beneficial to exclude NTM pulmonary disease as early nodular bronchiectatic changes often are not seen on standard radiographs.
Anyone who persistently or intermittently produces sputum who has an underlying lung disease is at risk of developing an NTM infection. Recurrent pneumonia is a big red flag for me. Since NTM live in the alveolar macrophages, NTM lung disease will make a patient more prone to the usual types of pneumonia. If you have a patient on their second or third admission for pneumonia, add an acid-fast bacillus (AFB) sputum culture. Keep NTM in mind, and check the cultures more than once. Know the nonspecific symptoms, and know that a chest X-ray may not show mild disease.
Our first principle in successfully diagnosing NTM infections is frequent bacterial and AFB sputum cultures in those patients with both symptoms and imaging changes consistent with disease. We want to know what is growing in a patient’s lungs over time. If obtaining sputum is not possible during a clinic visit, we send our patients home with a labeled sputum cup, and they drop off a sample at their convenience. For patients who don’t make sputum easily, our respiratory therapists will help obtain an induced sputum sample which can help avoid a bronchoscopy. We look for trends over time in the microbiology of each patient’s airways and tailor antibiotic regimens to specific organisms.
Advertisement
We also place a very strong emphasis on designing and implementing an aggressive airway clearance regimen, even for patients with mild NTM infection. We utilize a combination of inhaled and external clearance mechanisms, from bronchodilators and hypertonic saline through a nebulizer to acapella® Vibratory PEP and high-frequency chest wall oscillation devices (commonly referred to as “VEST”). Our respiratory therapists will help educate on other modalities of airway clearance such as huff coughing. We pay special attention to our patients whose COPD or asthma medications may actually impair airway clearance and optimize regimens accordingly. Pulmonary rehabilitation and patient education from respiratory therapists also play critical roles in successful long-term treatment.
As a Center of Excellence for bronchiectasis, we diagnose and treat many patients with NTM pulmonary infections. We have a multidisciplinary group of physicians and surgeons focused on both the lung disease and the infection by ensuring an optimal airway clearance regimen in addition to adherence to guideline-based antibiotic therapy. To refer a patient to our center, call 216.445.3082.
Dr. Khabbaza is staff in the Department of Pulmonary Medicine.
Advertisement
Advertisement

Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program