Biomechanics better than patellar tendon

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/96bf5a1b-40b3-4ec4-a0b2-18868917df77/ACL-jpg)
Torn ACL
The optimal tendon for an anterior cruciate ligament (ACL) autograft is still up for debate. Results from the Multicenter Orthopaedic Outcomes Network (MOON) support use of the patellar tendon, especially in young athletes and patients with high-grade laxity. The hamstring tendon is another popular option.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But Cleveland Clinic orthopaedic surgeon and sports medicine specialist Michael Scarcella, MD, says the quadriceps tendon deserves more consideration. While a robust tendon — a good source for an ACL autograft — the quadriceps tendon hasn’t been used or researched as much as other graft sources. In 2010 only 2.5% of ACL reconstructions were performed with the quad tendon. By 2014 the number had increased to 11%, according to a study in Knee Surgery, Sports Traumatology, Arthroscopy. An informal survey of surgeons at a recent national meeting found that quad graft use may be closer to 20% in primary ACL reconstructions.
“The quad tendon’s popularity is slowly increasing,” says Dr. Scarcella, who was introduced to the technique as a surgeon in the U.S. Navy. “After learning from one of my partners who had been using quad tendon autografts for years, I took the plunge and tried the technique on a patient referred to me for revision ACL. It had good results, so I started using quad tendon autografts for primary ACL reconstructions too. Those patients had less postop pain, less longer term anterior knee pain and less numbness. It seemed like they were recovering faster and moving their knees earlier, which was important for an active duty population.”
When Dr. Scarcella joined Cleveland Clinic in 2020, he brought his experience with the technique. Since then, Cleveland Clinic surgeons have been using quad tendon autografts more routinely, including for primary reconstruction.
Compared to patellar tendons, quad tendons offer a thicker graft with more favorable tensile properties, including:
Advertisement
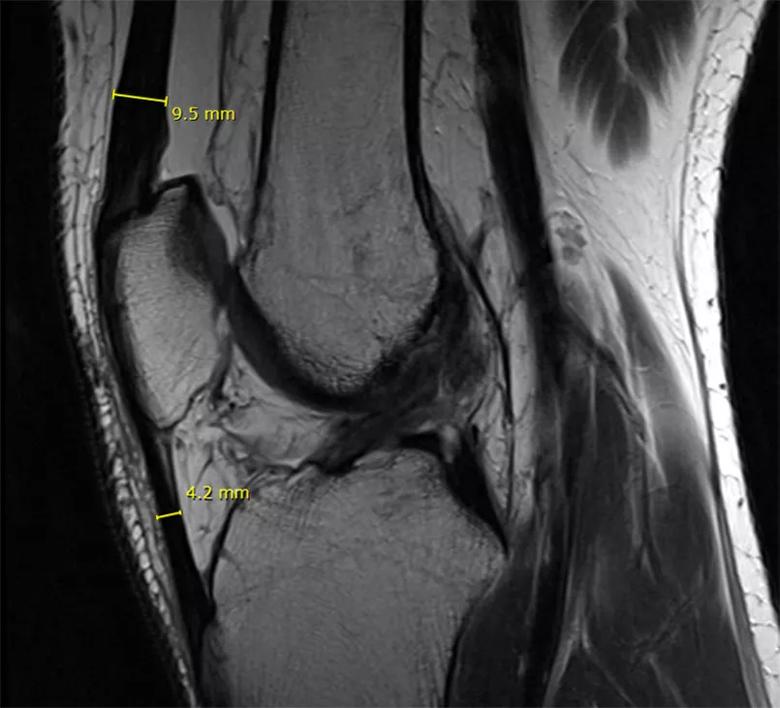
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e4bac4fe-440e-4d63-981e-5ba36f1ecf78/patella-tendon-INSET_jpg)
MRI demonstrating potential thickness of quad and patellar tendon grafts. Quad tendon thickness = 9.5 mm. Patellar tendon thickness = 4.2 mm
In addition, studies of quad tendon reconstruction have reported less anterior knee pain and numbness at 55-month follow-up, but equivalent stability and functional outcomes compared to patellar tendon reconstruction.
That’s not to say that quad tendon autografts are right for all patients. Graft choice should be individualized, based on imaging and a discussion of the patient’s goals and concerns, says Dr. Scarcella. History of tendonitis or tendonosis in any potential graft tissue is cause to rule it out as a graft option.
For surgeons considering use of quad tendon autografts for ACL reconstruction, Dr. Scarcella recommends these tips:
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/810adecd-ae6e-4430-8d66-373b0c959548/prepped-graf-INSET_jpg)
Prepped graft, 10 mm thickness.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e7eb2a33-47cb-4dfe-b06c-27521ae099cc/incision-INSET_jpg)
Harvest incision, 2 cm within natural skin crease.
Over the last five to 10 years, surgical instrumentation has made harvesting tendon autografts easier and more precise.
“We’re getting accurate sizes and quality length, and we have good devices to attach and suspend the graft in place while it heals into or around the bone tunnels,” says Dr. Scarcella. “Quad tendon grafts are strong, reliable, readily available and a lot thicker than the patellar tendon — and can be harvested through a tiny incision. Outside of the biomechanical advantages of the graft and the reduced complications, the smaller harvest site can lead to a more aesthetically pleasing postoperative appearance.”

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8f126e2d-a9e4-4c94-9119-8baee995d95f/Scar-INSET_jpg)
Seven weeks after quad tendon ACL reconstruction.
Advertisement
Advertisement
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
Percutaneous stabilization can increase mobility without disrupting cancer treatment