Essentials of cerebral venous sinus thrombosis from a neurointensive care/stroke specialist
With the federal pause lifted on U.S. administration of the Johnson & Johnson (J&J) COVID-19 vaccine, new vigilance is in order for symptoms of the rare condition that led the Centers for Disease Control and Prevention (CDC) to temporarily halt use of the vaccine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The pause was prompted by six known cases of cerebral venous sinus thrombosis (CVST) with thrombocytopenia that occurred two to three weeks following receipt of the J&J vaccine. On April 23, the CDC’s Advisory Committee on Immunization Practices reported that the number of known cases had risen to 15 as of April 21, including three deaths. Twelve of the 15 cases have been CVST, with three involving other forms of thrombosis; all patients have had thrombocytopenia. All cases have been in women, and 13 of the 15 patients have been between ages 18 and 49.
“The most common symptom is a dull, pounding headache that becomes severe enough to prompt the individual to seek emergency care,” says Pravin George, DO, a neurointensive care and stroke specialist with Cleveland Clinic’s Neurological Institute.
While headache is very common in the general public, Dr. George says this type of headache stands out. “It alarms people who may not normally have headaches as well as those who suffer from migraines, because it may cause a headache different than a normal migraine,” he explains.
All of the six initial CVST patients who received the J&J vaccine reported headaches. Additionally, all experienced symptoms consistent with stroke or deep vein thrombosis. Some also reported bruising, vomiting or loss of consciousness — symptoms of increased pressure in the brain.
“When we see CVST outside the vaccine context, patients are usually females ages 18 to 40,” notes Dr. George. “They develop a headache, it worsens and then they can even develop seizures. Some also report blurred vision or nausea.”
Advertisement
Seizure is the second most common symptom, although it was not seen in the initial six CVST patients who had received the J&J vaccine.
CVST is rare, representing less than 1% of all strokes. Risk factors include malignancy, prothrombotic conditions, oral contraceptive use, infection and pregnancy/postpartum status.
The condition is three times more common in females than males. “There is some indication that estrogen and progesterone may play a role,” says Dr. George. “In the cases among J&J vaccine recipients, we think the vaccine may cause an immune reaction that makes the individual prone to developing clots.”
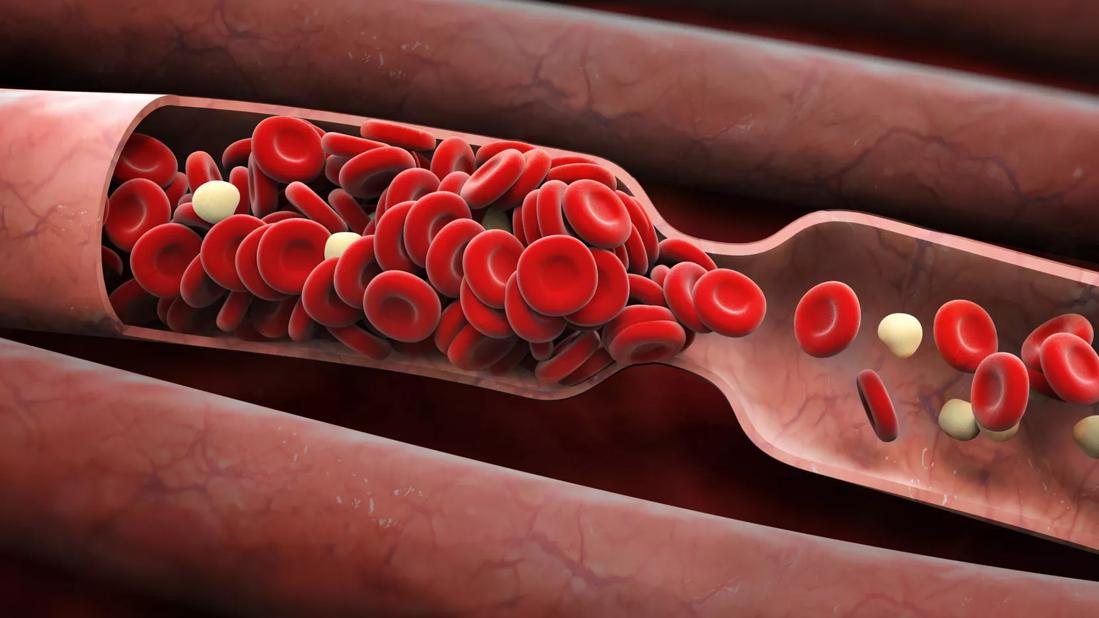
CVST occurs in the smaller cortical veins and spreads to the sinuses, which drain into the jugular veins. If clotting is not stopped early, any section of the venous system can become blocked. “Arteries continue feeding blood into the brain, and with no way for the blood to exit, the buildup of pressure can cause brain hemorrhages,” says Dr. George.
Four of the initial six CVST cases in J&J vaccine recipients involved intracerebral hemorrhage. Additionally, three cases involved deep vein thrombosis or pulmonary embolism, indicating a hypercoagulable state.
Patients who experienced CVST following the J&J vaccine also developed thrombocytopenia, a condition not typically associated with CVST, since thrombosis typically does not occur in the presence of low platelets.
For individuals with symptoms that raise suspicion for CVST — i.e., unusual new-onset headache, seizure, symptoms of stroke, abdominal or leg pain, blurred vision, nausea or vomiting — within two or three weeks of receipt of the J&J vaccine, Dr. George recommends the following management steps:
Advertisement
Despite concerns about the safety of the J&J vaccine, Dr. George stresses the importance of getting vaccinated against COVID-19.
“Widespread vaccination of all eligible individuals will move us toward herd immunity,” he says. “The CDC’s Advisory Committee on Immunization Practices has determined that the J&J vaccine’s benefits outweigh its risks, and no safety concerns have arisen with either the Pfizer-BioNTech or the Moderna vaccines across tens of millions of doses administered.”
He also reminds providers of the need to track potential complications associated with any of the COVID-19 vaccines by reporting them to the national Vaccine Adverse Event Reporting System at vaers.hhs.gov.
Advertisement
Advertisement

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition

As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19