By Gian Novaro, MD, Director, Echocardiography, Robert and Suzanne Tomsich Department of Cardiology Cleveland Clinic Weston Hospital
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is reprinted from Cardiac Care Publication News From Cleveland Clinic in Florida.
Bicuspid aortic valve (BAV) disease is one of the more common congenital heart conditions encountered in clinical practice. The estimated prevalence in the general population is 1-2%, with a predominance in males at a 4:1 ratio. Most BAV disease occurs in isolation, although a small fraction of patients may have other associated congenital heart diagnoses. It is important to recognize the presence of BAV disease as most patients will suffer related complications in their lifetime. Our team at Cleveland Clinic Weston Hospital in Florida is proud to be among the leaders in our state in the field of BAV disease research.
BAV disease is a malformation resulting in an aortic valve with only two leaflets, or cusps, compared to the three found in a normal aortic valve. Because of the structural abnormality the valve is subject to greater mechanical trauma over time. Most commonly, the valve accumulates calcium and cholesterol deposits, which, over time, limits its mobility and leads to stenosis. This condition usually begins to affect patients in their 50s and 60s. In about 20% of BAV disease cases, the valve opens but fails to close properly, leading to aortic valve regurgitation, or backflow, into the left ventricle. When present in isolation, this condition often presents in younger patients in their 30s and 40s.
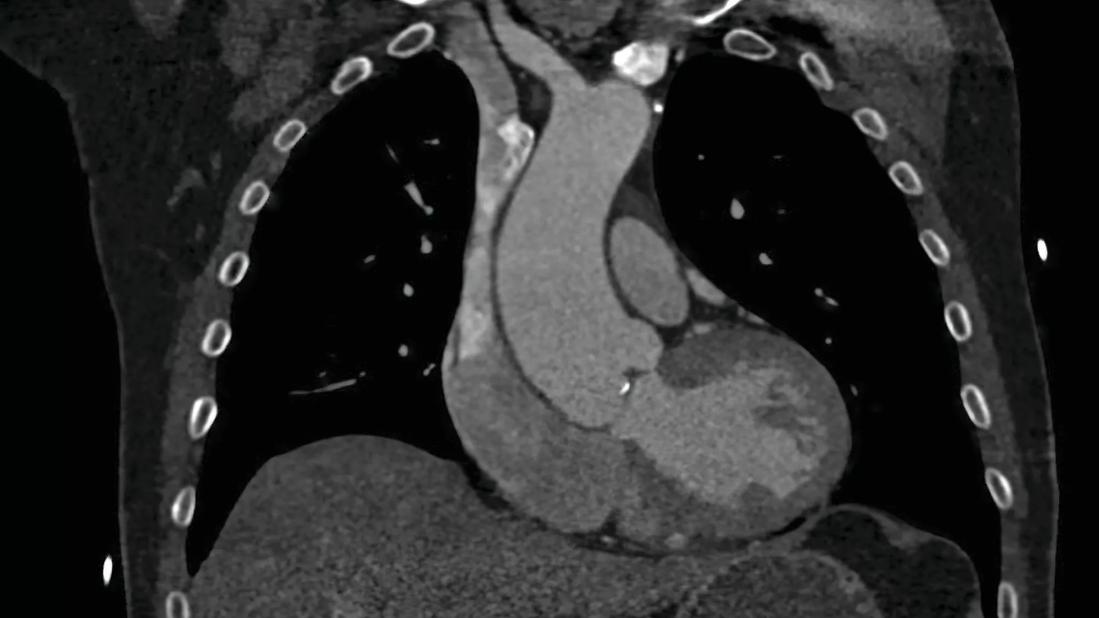
About 40 to 50% of BAV disease patients develop a dilatation of the aortic root and ascending aorta. In less than half of these cases, an aortic aneurysm is present, requiring ongoing surveillance and possible eventual repair. The aortic segments of dilatation can vary in BAV disease patients with the mid ascending region being the most common. Other phenotypes of aortic aneurysm exist, including aortic root predominant and a diffuse dilatation pattern. Rates of aortic growth vary but are unreliable to predict an upcoming aortic event. The current recommendation for elective aortic repair is an aortic diameter of 50-55 mm, with a threshold based on risk factors of family history of aortic instability or signs of rapid aortic growth.
Advertisement
BAV disease cases often require referral to cardiac imaging specialists who bring experience in complex valve and aortic diseases. Transthoracic echocardiography (TTE) is the standard diagnostic test when evaluating patients with a suspected aortic valve abnormality. TTE allows for accurate assessment of aortic valve anatomy and function, and the potential associated condition of aortic dilatation. Left ventricular size and function are defined by 2D and 3D volumes and ejection fraction. Transesophageal echocardiography can be used to complement TTE in cases where the diagnosis is in question or when the valve lesion requires more quantitation. In BAV disease patients with related aortic dilatation or aneurysm formation, we obtain a CT angiogram or cardiac MRI to better define aortic anatomy and baseline dimensions.
Once a case of BAV disease is diagnosed, it is important to recognize that among families, as many as 10-15% of first-degree relatives may harbor BAV disease. Because of this prevalence, the screening of first-degree family members is recommended. Screening usually is done with a TTE to assess aortic valve anatomy and its function, as well as screen for dilatation of the ascending aorta.
Decision-making and management strategies in BAV disease patients, particularly those with aortic aneurysm, can be challenging and often require a second opinion. Referral to a comprehensive heart valve center is beneficial when the time comes to consider treatment options. Cleveland Clinic Weston Hospital’s multidisciplinary heart valve team offers the expertise and experience needed for tailoring the appropriate treatment strategy for each patient and includes advanced cardiovascular imaging specialists, cardiologists and interventional cardiologists specializing in aortic valve disease, and surgeons with extensive experience repairing cardiac valves.
Advertisement
For younger patients with BAV disease with aortic regurgitation, the option of valve repair is available. Carefully selected patients with pure aortic regurgitation and preserved valve architecture often can be successfully repaired and spared from a valve replacement. If an aortic aneurysm is present, the surgery may involve ascending aortic repair in combination with valve repair, referred to as a valve-sparing approach. For those with mainly aortic valve stenosis, the options of surgical valve replacement versus transcatheter aortic valve replacement (TAVR) exist. Patient-specific risk factors, anatomic considerations, age, and preferences are taken into consideration when determining the candidacy of a surgical approach versus TAVR.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.