Phase 3 trial found no survival differences between weekly or biweekly doxorubicin/cyclophosphamide or between weekly or biweekly paclitaxel
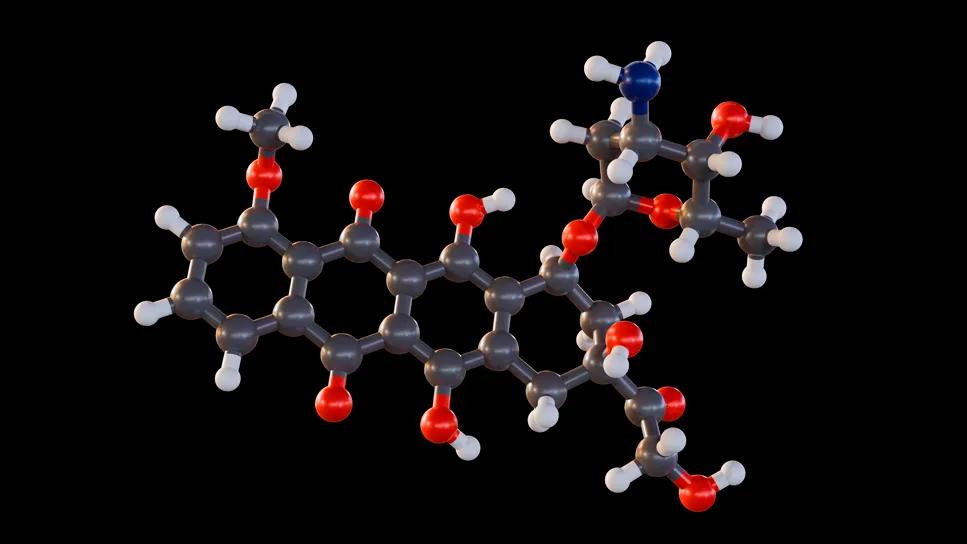
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f3f33c94-797f-4fa6-b485-1a24223cc1f2/alternative-dose-schedules-early-brca-2152418318)
rendering of Doxorubicin molecules
The treatment landscape for early breast cancer continues to evolve, with chemotherapy remaining a cornerstone for high-risk cases despite advancements in targeted therapies. The S0221 trial, conducted by the National Clinical Trials Network (formerly the North American Breast Cancer Intergroup), sought to optimize chemotherapy dosing schedules—and improve outcomes—for patients with node-positive or high-risk node-negative breast cancer.
Spanning more than a decade, the study compared weekly and biweekly administration of doxorubicin/cyclophosphamide and paclitaxel, assessing disease-free survival (DFS), overall survival (OS) and toxicity profiles. With over 3,000 participants, including a subset of 578 patients enrolled under a revised protocol, the trial provides critical insights into the efficacy and tolerability of these schedules, offering guidance for tailoring treatment to individual patient needs.
During the 2024 San Antonio Breast Cancer Symposium (SABCS), Azka Ali, MD, an oncologist with the Department of Hematology and Medical Oncology at Cleveland Clinic, presented updated survival outcomes from the original protocol as well as the first report on the additional arms under the revised protocol.
“While we have seen ongoing treatment advancements, including the introduction of targeted therapies, in breast cancer, chemotherapy still plays an important role for many early high-risk patients. And the question has been, ‘what is the right schedule for chemotherapy?’” notes Dr. Ali.
“Ideally, we want to find the schedule that gives us the most effective response with the least amount of toxicity,” she continues. “In S0221, we observed no significant differences in disease-free or overall survival between the treatment schedules, suggesting that either anthracycline or paclitaxel regimens can be recommended, with the choice depending on factors such as toxicity, cost or patient preference rather than on differences in efficacy.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This phase 3, randomized trial explored weekly doxorubicin/cyclophosphamide (AC) plus granulocyte colony stimulating factor (GCSF) versus every two weeks (Q2W), followed by paclitaxel administered Q2W or weekly for 12 weeks as adjuvant therapy for patients with node-positive or high-risk node-negative breast cancer.
Between December 2003 and November 2010, 2,716 patients were randomized in a 2x2 factorial design to the following groups: 1) 15 weeks of weekly AC versus six cycles of Q2W AC, and 2) weekly paclitaxel versus Q2W paclitaxel with GCSF support, corresponding to arms 1–4.
At the first interim analysis in 2010, researchers determined that weekly AC was unlikely to offer any superiority over every-two-week doxorubicin/cyclophosphamide. As a result, accrual was suspended, and the trial protocol was modified and reopened.
Under the revised protocol, all study participants, including an additional 578 patients, received four cycles of every two-week AC and were randomly assigned to one of the following paclitaxel regimens: paclitaxel 175 mg/m² intravenously on day 1 with pegfilgrastim 6 mg subcutaneously on day 2, repeated every two weeks for six cycles, or paclitaxel 80 mg/m² weekly for 12 weeks.
At a median follow-up of 12.1 years, Dr. Ali and colleagues observed no significant differences in disease-free or overall survival between the four treatment arms in the original protocol. When stratified by disease subtype, patients in the HER2-positive group had the highest 10-year DFS rate (77.7%) compared to the HR-positive/HER2-negative (70.6%) and HR-negative/HER2-negative (70.3%) cohorts.
Data showed that the HER2-positive group also had the highest 10-year overall survival rate (82.3%) in comparison to HR-positive/HER2-negative (78.1%) and HR-negative/HER2-negative (74.9%) patients.
Among the 578 patients who received AC for four cycles and randomized to weekly versus Q2W paclitaxel, no significant differences were found in disease-free or overall survival. Additionally, investigators reported no notable difference in the 10-year DFS rate between the original (71.3%) and revised (74.4%) protocols.
The investigators also stratified patients by sex (23 men) and race (379 Black patients). Women showed superior DFS and OS when compared to their male counterparts; however, Dr. Ali notes that these results should be interpreted with caution due to the small number of men and wide confidence intervals. The study results revealed that Black patients had worse DFS and OS, with a 10-year DFS rate of 64.2% (Black) versus 72.8% (other races), and a 10-year OS rate of 70.4% (Black) versus 79.0% (other races).
In terms of toxicity, cardiac toxicity profile appears similar across the six arms, according to the study authors, who also reported that the weekly AC schedule was associated with higher rates of skin toxicity (15.7–16.1%) when compared to the other arms (2.4–4.0%).
No differences in infectious risk or metabolic changes were observed; however, there was more neuropathy in patients treated with paclitaxel every two weeks compared to weekly. It should also be noted that in S0221, patients received paclitaxel every two weeks for a total of six weeks (versus four cycles).
Based on the final analysis of S0221, Dr. Ali and colleagues conclude that there is no difference in efficacy in any of the four treatment arms of anthracycline and/or taxane schedule or in the two arms of the revised protocol. Additionally, weekly anthracycline for 15 weeks does not improve efficacy and, therefore, they do not “strongly advocate for that dosing schedule,” Dr. Ali says.
“As for whether you should give the paclitaxel portion every two weeks or weekly, the individual needs and preference of the patient should be taken into account,” she advises. “For patients who live far away or are younger and can tolerate the dose dense schedule every two weeks, the every-two-week regimen may be preferred.”
“However, for older patients, the weekly paclitaxel regimen may be more suitable due to its lower dose and potentially a more favorable tolerance potential. Ultimately, the decision should be based on patient preferences and potential toxicity,” Dr. Ali concludes.
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer
Reconsidering axillary lymph node dissection as well as depth of surgical margins
Ultra-Hypofractionated Whole Breast Irradiation and Partial Breast Irradiation Reduce Many Toxicities
Best practices for reducing toxicities
Partnerships with local social service agencies key to program success
Ongoing clinical validation refine breast cancer risk substratification
Findings strengthen evidence for risk-reducing procedures