Distinct baseline immune profiles can predict response and resistance to different types of CAR-T cells.
Researchers at Cleveland Clinic Research have identified distinct predictors of response or resistance to different types of chimeric antigen receptor (CAR) T-cell therapy in people with relapsed/refractory B-cell non-Hodgkin’s Lymphoma (NHL), potentially leading to better personalization of treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although CD19-directed CAR T-cell therapy has revolutionized the treatment of many blood cancers, fewer than 40% of patients experience long-term remission.
Post-infusion parameters such as CAR T-cell persistence, certain phenotypes, tumor burden and the immune microenvironment are correlated with CAR T-cell efficacy, but there have been no reliable baseline or pre-lymphodeletion biomarkers to predict clinical response.
A new study presented at the American Society of Hematology (ASH) meeting shows that distinct baseline immune and plasma protein signatures can predict response and resistance to CAR T-cells that were engineered with 4-1BB, a signaling molecule that activates the T-cell after it binds to the tumor cell.
Importantly, those biomarkers differ from predictors of response to CAR T-cells made with a different signaling molecule, CD28. Some of those predictors were also identified in a separate study presented at the ASH meeting.
The distinctions are important because the current commercially available CAR T-cell products for B-cell NHL differ in the activation molecules used in their manufacturing processes. Axicabtagene ciloleucel incorporates a CD28 costimulatory domain, whereas tisagenlecleucel and lisocabtagenemaraleucel are both engineered using a 4-1BB costimulatory domain.
In general, CD28 provides stronger, faster activation, leading to rapid proliferation but with slightly more toxicity, whereas 4-1BB is slower and provides longer-lasting and more resilient CAR T cells with lower toxicity. The choice of which product to use in a given patient is currently based on those properties, along with clinical characteristics.
Advertisement
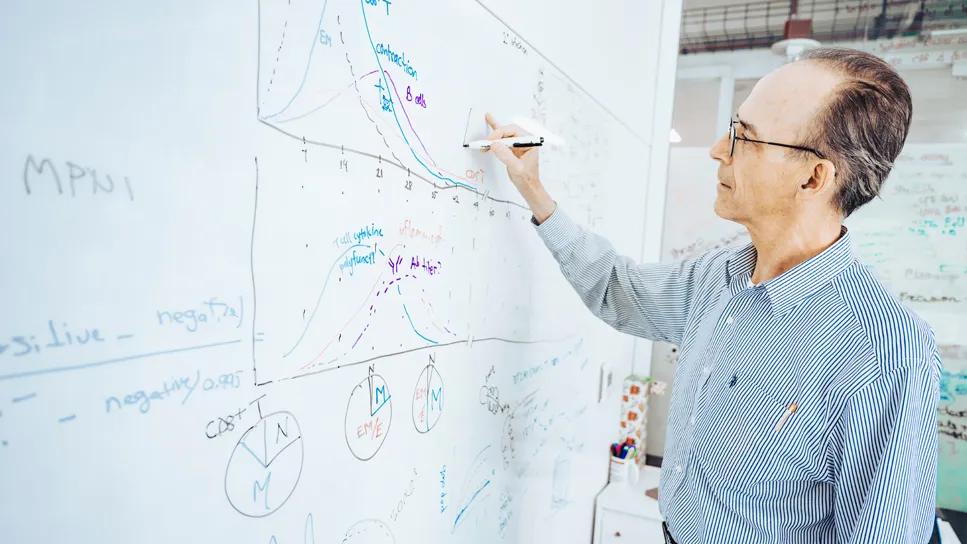
“We confirmed that a particular T-cell subset present in the starting material is very important for the therapeutic outcome. It suggests that we can pre-select the cells that are predicted to drive the response. We can isolate those and make responses better,” said lead investigator J. Joseph Melenhorst, PhD, Director of Cell Therapy and Immuno-Engineering Program and Professor at Cleveland Clinic's Lerner College of Medicine.
“Until now, it was not clear that the reasons for failing or responding to CAR T-cell therapy differed between the different CAR T-cell types,” says study co-investigator Paolo Caimi, MD, Associate Bone Marrow Transplant Director for Cellular Therapy. Going forward, we hope to use that information to help better personalize the choice of treatment for a given patient.”
In a phase 1 clinical trial, 26 patients with relapsing/refractory B-cell NHL received CD19 CAR T-cells manufactured using 4-1BB. Of those, 19 patients achieved a complete remission at six months while three achieved partial remission. The responders showed a significantly higher frequency of early memory T cells, while non-responders had higher proportions of effector memory and terminal effector cells.
Consistent with previous findings in B-cell acute lymphoblastic leukemia, T cells with type 2 function were significantly enriched in the responders. This was the first such finding in NHL.
At the same time, regulatory T cells were reduced in the non-responders. Proteomic analysis at baseline and post-infusion also identified differences in responders and non-responders.
Advertisement
In a separate study involving 60 patients who were heavily pretreated for large B-cell lymphoma received axicabtagene ciloleucel. At six months, the overall response rate was 56.7% and the complete response rate was 57.6%. One specific baseline central memory CD8+ T-cell signature was found to strongly predict resistance to CD28-based CAR T-cell therapy in NHL, contradicting prior thinking that memory T cells are always beneficial in CAR T-cell therapy.
In the non-responders, pre-infusion CD8+ T cells show type 2 polarization, which is thought to reflect tumor-driven adaptation that impairs cytotoxicity. This contrasts with the group’s previous findings in the 4-1BB-based CAR T-cell product tisagenlecleucel in leukemias, where memory function and type 2 CAR T-cells are necessary for long-term efficacy and persistence.
“The biomarkers could not be any more different between the two CAR T types,” Dr. Melenhorst says. “We now believe that early identification of these phenotypes at leukapheresis may enable better patient stratification and guide use of alternative products to maximize therapeutic success.”
Under Dr. Melenhorst’s leadership, Cleveland Clinic Research is now setting up an in-house point-of-care manufacturing center for CAR T-cell therapy. The center was approved to construct a Good Manufacturing Practice (GMP) facility required for developing and processing cellular products, which will be used in future clinical trials. “Our next step is to use our findings to produce more effective CAR T-cells,” Dr. Melenhorst says.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors