Clinicians share practices to streamline initiation of care

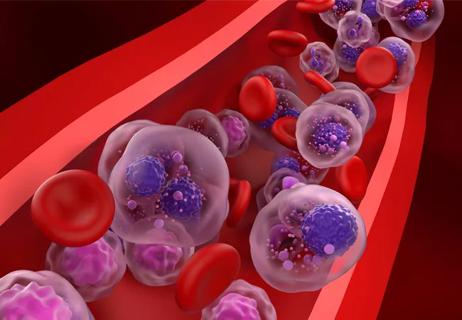
For patients newly diagnosed with multiple myeloma, time is of the essence for initiating treatment. Promptly starting antimyeloma medications such as lenalidomide helps mitigate the risk of myeloma-related bone fractures, kidney damage and disease progression. Yet a recent study found that the median time from the date of diagnosis to initial prescription fill was 28 days.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A team of researchers secured a National Cancer Institute grant to determine modifiable factors that influence time to treatment. “We wanted to find actionable ways to support prompt initiation of therapy,” says Hamlet Gasoyan, PhD, study co-author and an investigator at Cleveland Clinic Center for Value-Based Care Research.
The study included a retrospective analysis of 720 adult patients newly diagnosed with multiple myeloma between January 1, 2017 and December 31, 2021. The study examined the time it took to fill an oral antimyeloma treatment (excluding corticosteroids) from the date of diagnosis. Researchers also looked at factors such as age of diagnosis, type of insurance, and whether the diagnosis occurred during an inpatient admission.
During the study follow-up, 543 patients filled a prescription for an oral antimyeloma medication other than corticosteroids. Among those, the median time to initial prescription fill was 28 days. For a quarter of patients, the time to treatment with immunomodulatory drugs was ≥2 months. Researchers also found there were notable differences in time-to-treatment among Black patients, patients who were older at the time of their diagnosis as well as patients who were first diagnosed while in the hospital.
Key barriers that impede swift time-to-treatment include:
Advertisement
Even for patients with private insurance, they may still be responsible for a sizeable portion of the cost of the medication. For example, in 2018, the median out-of-pocket cost during the first year after myeloma diagnosis was $3,711 for privately insured patients and up to $5,623 for patients with high-deductible health plans.
“Assessment for eligibility for external funding goes smoother with an in-house specialty pharmacy as opposed to an external pharmacy,” explains Joslyn Rudoni, PharmD, BCOP, a clinical pharmacy specialist in the myeloma clinic at Cleveland Clinic. “It is exponentially more difficult to communicate directly with personnel at external pharmacies to facilitate timely prior authorization and triage billing issues, such as assessment of affordability of patient copays and coordination of grant applications or patient assistant programs, all of which our internal specialty pharmacy tackles seamlessly on behalf of our providers to streamline the process. The communication barriers with external pharmacies make the ability to expedite prescriptions uniquely challenging and often unattainable."
Advertisement
Alleviating these delays is a complex process but is not insurmountable. Several practices that could have a profound difference for patients include:
Providing specialty pharmacy capabilities internally. Cleveland Clinic built its own in-house specialty pharmacy that is now authorized to dispense these medications, as long as the patient’s insurance allows it. “We feel that having an in-house specialty pharmacy we can communicate with directly will make a big difference for patients,” says Dr. Valent.
Accelerating treatment initiation and prescriptions for newly diagnosed patients in the inpatient setting. In some cases, the available medications, including bortezomib, cyclophosphamide, dexamethasone and in rare instances daratumumab, can be started during the inpatient stay. At the same time, the hospital can start the process of the lenalidomide prescription and work with the specialty pharmacy to expedite the drug availability. (Note: Daratumumab has a high cost and may not be reimbursed when administered during an inpatient stay.)
Improving appointment access. Once diagnosis is established, patients are given an appointment as quickly as possible to discuss the treatment strategy. “During the same visit, we complete the diagnosis process, including staging workup, education about medications and side effects,” says Faiz Anwer, MD, co-author of the study and a hematologist at Cleveland Clinic Cancer Institute. “We may also prescribe steroids that can be started the same day or next day, so that even if there’s a delay in other medications, the patient is able to start this treatment swiftly to gain anti-myeloma and anti-inflammatory effects.”
Advertisement
Supporting common-sense policies. Encouraging insurance carriers to provide coverage for cancer therapies, regardless of whether it’s intravenous or oral, could relieve patients of the copay burden they currently face.
Providing patient navigators. “When patients are left to deal with the administrative burden themselves, they may face more of a delay,” says Dr. Gasoyan. It’s estimated that there are thousands of people across the country who don’t have access to patient support systems, yet these are essential to helping patients through these complex administrative issues.
For example, centers like Cleveland Clinic have teams that help patients access copay assistance programs; apply for Medicaid, the Hospital Care Assurance Program or other appropriate insurance; and more. “We make it a priority to ensure patients receive treatment and remove barriers to getting the medication they need,” says Dr. Anwer.
“It’s been a very exciting decade of scientific advances in multiple myeloma treatment, and survival has improved significantly,” says Dr. Gasoyan. “With that, it becomes even more important to understand the barriers to timely initiation of care.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Phase 2 study brings pivotal advances in treatment efficacy and safety for the most challenging-to-treat population

Making sense of the fast-moving treatment landscape

Explaining common misconceptions about chimeric antigen receptor therapy

Prediction and bioinformatic data could prove valuable for therapeutic interventions targeting this malignancy

Findings from large database important to inform clinical practice

Study of 401,576 patients reveals differences in cancer burdens as well as overall survival
Despite sicker patients, response rates of teclistamab in a real-world study were similar to those from a pivotal clinical trial