Minimal residual disease testing shows promising results
After receiving myriad treatments since first being diagnosed with multiple myeloma in 2006, a 79-year-old man presented in August 2021 with slowly increasing M-spike numbers. He had exhausted other treatment options, and was seen at Cleveland Clinic’s Taussig Cancer Institute for consideration to receive chimeric antigen receptor (CAR) T-cell therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In September 2021, the patient was approved for idecabtagene vicleucel (ide-cel) CAR T-cell therapy, a treatment that resulted in a deep, durable response. “It’s important to note that being older is not a contraindication for CAR T-cell therapy,” says Jack Khouri, MD, a hematologist/oncologist with the Taussig Cancer Institute. “Our patient was very fit, and was a good candidate for this therapy.”
Like many patients with multiple myeloma, the patient had been through a long and arduous journey battling the disease. He had received more treatments than most patients, recalls his primary hematologist, Jason Valent, MD, who has been caring for him since 2011.
Twice over the course of the disease, the patient became critically ill due to disease progression, and was nearly out of options when a new therapy was FDA approved. The first was pomalidomide, which he received when it was first approved in 2013. He responded very well to this treatment for roughly two years. At that point, his disease progressed, and he needed a new treatment. Daratumumab was FDA approved in November 2015, and Dr. Valent initiated him on this treatment within weeks. He was put on multiple medications sequentially along with daratumumab. Of the years this included cyclophosphamide, bortezomib and ixamobil.
In 2021 and 2022, the FDA approved two CAR T-cell therapies for treating multiple myeloma in patients who have experienced relapse after at least four prior lines of therapy.
With this treatment, the patient’s own cells are engineered to target a specific antigen. Intended to be a “living drug” that remains in the body fighting cancer, CAR T-cell therapy is a one-time therapy. Though CAR T-cell therapy is not generally curative for patients with multiple myeloma, it can provide remission for months and sometimes years. This can free patients from the burden of receiving regular treatment. For someone who’s been on treatment continuously since 2006, that held a great deal of appeal.
Advertisement
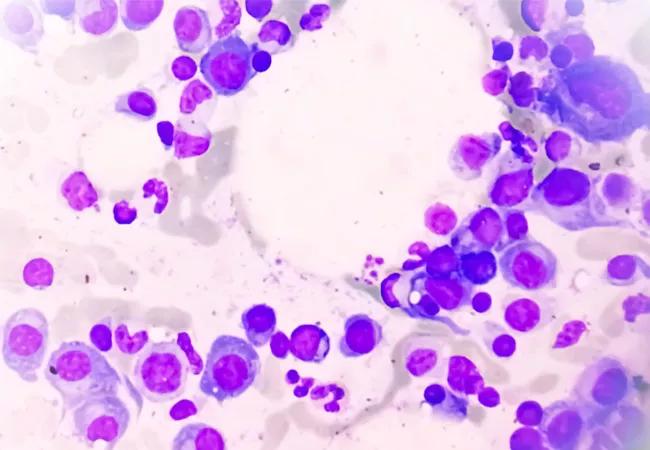
The workup for CAR T-cell therapy includes a bone marrow biopsy, an echocardiogram, bone imaging, liver and kidney function tests as well as a review of the patient’s medical history. In this case, the patient was found to have adequate organ function to proceed. He had a history of limited prostate cancer years before, and that had resolved through radiation. Other than having hypertension and high cholesterol, he was in good health.
Based on this, Dr. Khouri proceeded to rapidly seek approval for the patient to proceed with CAR T-cell therapy.
Since his abnormal protein numbers continued to accelerate, the patient was administered a combination of carfilzomib, pomalidomide and dexamethasone up until two weeks prior to having his cells collected for CAR T-cell therapy. After his cells were collected and in the manufacturing process, he continued on the three-drug regimen to keep the disease in check and to help minimize the disease burden going into CAR T-cell therapy.
He then began several days of lymphodepleting chemotherapy. “The purpose of this chemotherapy is to make room for the incoming T-cells to grow in the body,” explains Dr. Khouri. “The patient tolerated this process well with no side effects.”
From there, the patient was admitted to the hospital in preparation for the CAR T-cell infusion. He stayed in the hospital for a week of close observation after the cells were infused. A highly specialized team of hematologists and nurses cared for the patient in the Bone Marrow Transplant unit of the Clinic for the duration of his treatment.
Advertisement
Fortunately, the process went very smoothly. In a certain percentage of patients, cytokine release syndrome or neurotoxicity can occur after CAR T-cell therapy, but the patient had neither. In addition, his blood counts recovered quickly, with no need for transfusions. “Roughly 60-70 percent of patients need some kind of transfusion support for the first two months after treatment,” says Dr. Khouri. “He was one of the 30-40 percent who did not need that at all.”
The care team saw the patient in the clinic weekly for the first month after hospital discharge to check his overall health as well as his blood counts. As with all patients receiving CAR T-cell therapy, he needed a 24/7 caregiver to be with him at all times for the first month after the infusion to ensure he wasn’t experiencing neurotoxicity such as confusion or seizures once he was at home. In this case, the patient’s wife fulfilled that role. His recovery went well, and he had no toxicities, infections or hospitalizations following treatment.
Blood and urine tests performed after treatment demonstrated that the patient had achieved a stringent complete response. The care team then performed minimal residual disease testing, and was thrilled to find that even for that sensitive measure, the patient was negative for identifiable cancer cells. “He achieved a very deep response from his CAR T-cell therapy, and that is a good marker for long-term outcomes,” says Dr. Khouri.
The patient now has an exceptional quality of life. He is back to enjoying golf with his friends, mowing the lawn at his daughter’s house and spending time with his wife of more than 50 years. “It’s a remarkable example of the tremendous impact cellular therapy can have,” says Dr. Valent. “I can’t believe how far he’s come.”
Advertisement
This case study illustrates the importance of engaging a CAR T-cell team early on if myeloma is beginning to progress – and not to rule out the treatment based on a patient’s age. “If a patient’s [protein] numbers are starting to elevate, that is the time to consider seeking an assessment to determine whether CAR T-cell therapy is the right option,” says Dr. Khouri.
Advertisement
Advertisement

Age alone should not rule out patients from potentially curative treatment

Higher type 2 immunity observed in persistent CAR T cells

Real-world study shows high response rates that are durable with commercial lisocabtagene maraleucel
Dispelling myths and sharing practical experiences

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Phase 2 study brings pivotal advances in treatment efficacy and safety for the most challenging-to-treat population

Early results show patients experiencing deep and complete response

Making sense of the fast-moving treatment landscape