New findings may lead to less-toxic tumor therapies
Traditional oncology treatments aim to kill cancer cells. But what if science could find a way to heal them instead? That’s the premise behind a new study designed to uncover the process by which healthy kidney cells mutate into kidney cancer. Researchers hope the findings can eventually be used to develop a new type of cancer therapy – one that aims to repair diseased cells rather than simply destroy them.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“When a patient comes in with a broken femur, we don’t remove it and ask them to get a new one – we fix it,” says Cleveland Clinic hematologist/oncologist Yogen Saunthararajah, MD of Taussig Cancer Institute. “But when a patient develops cancer, we routinely set out to destroy it because we just don’t know what else to do. Unfortunately, this traditional approach can cause collateral damage, including toxicity, and often fails to destroy the cancer.”
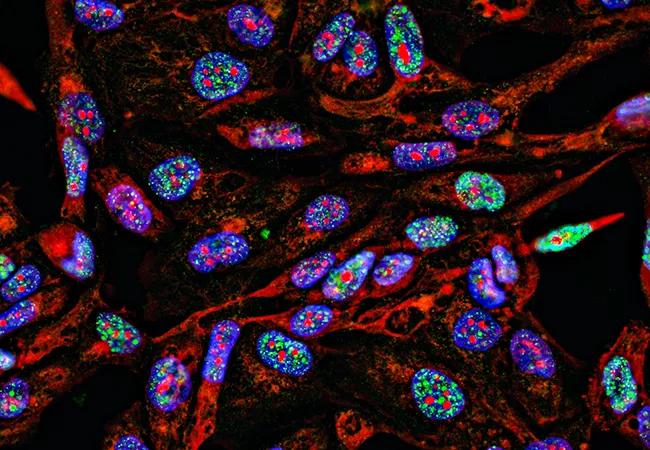
Recently published in the journal Cell Reports, Dr. Saunthararajah’s latest study evaluated the genesis of clear cell renal cell cancer, the most common subtype of kidney malignancy. Researchers began with the premise that all tissues undergo a normal process of replenishment and repair. It was hypothesized that cancer develops when something interrupts that process and causes cells that seek to replenish tissue to get “stuck.” Dr. Saunthararajah explains these cells “spin their wheels instead,” continuing to replicate at an intermediate stage in their journey.
Study researchers used mass spectrometry to analyze the larger machinery in which PBRM1, a gene shown to play an essential role in kidney cancer genesis, operates. Dr. Saunthararajah says that PBRM1 is a key component of a protein machine used to activate the genes that define a specialized kidney cell.
“Without PBRM1, the developing cell cannot turn on and focus on the specialized functions of a kidney cell; instead, it continues to focus on growing and dividing,” he says.
Advertisement
While it’s technically difficult to treat the problem by adding back missing PBRM1, therapy could involve inhibiting the enzymes that naturally oppose PBRM1, restoring balance and turning on specialized kidney cell fates, he notes.
“There is nothing inherently toxic about that approach,” says Dr. Saunthararajah. “That’s the significance of this finding; understanding at a molecular-machine level how a developing kidney cell becomes a cancerous cell opens the door to repair, allowing the cell to become what it was intended to become all along. These findings can help us develop new treatments that are very different from the ‘search and destroy’ approach seen with traditional cancer therapy.”
Dr. Saunthararajah’s research group previously showed a similar process at work in the development of liver and blood cancers. “We suspect that disruption to the machinery that developing cells use to turn on specialized tissue cell genes is a general theme in cancer genesis,” he says.
Investigators, which have already developed drugs that repair leukemia and blood cancers in accordance with this principle, are now working on similar therapies to combat solid tumor malignancies, such as kidney cancer.
“There’s a tendency to think that an idea has to be complicated to be good science, but our theory is actually quite straightforward,” says Dr. Saunthararajah. “Cells that are meant to replenish our tissues cannot complete their journeys because hundreds of specialized tissue genes are enzymatically ‘turned off.’ If you inhibit the unbalanced ‘off’ enzymes, you fix the cancer. It could be that simple.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors