Leveraging the prognostic significance of sentinel lymph node biopsy histologic patterns
Cleveland Clinic Cancer Center investigators have published a body of research that may herald an era of improved staging and risk stratification for patients with Merkel cell carcinoma (MCC), an aggressive and lethal form of skin cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The focus of their work is sentinel lymph node (SLN) biopsy, a technique increasingly used for MCC treatment planning but whose pathologic prognostic significance in patients without clinically evident positive nodes has been unclear.
Because MCC is uncommon, few studies have been done to evaluate the predictive value of the variable amounts and patterns of cancer cells detected in SLN biopsies from patients with the disease. Only 2,500 cases of MCC are diagnosed annually in the United States, but incidence is increasing. Eighty percent of MCC cases are caused by infection with a DNA oncovirus, Merkel cell polyomavirus; the remainder result from cumulative exposure to ultraviolet radiation.
Three recent studies by a multidisciplinary Cleveland Clinic Cancer Center research team shed new light on the potential value of SLN biopsy in MCC. Key members of the team are dermatopathologist Jennifer Ko, MD, PhD, medical oncologist Pauline Funchain, MD, and plastic surgeon Brian Gastman, MD, the Medical and Surgical Director of the Melanoma and High-risk Skin Cancer Program.
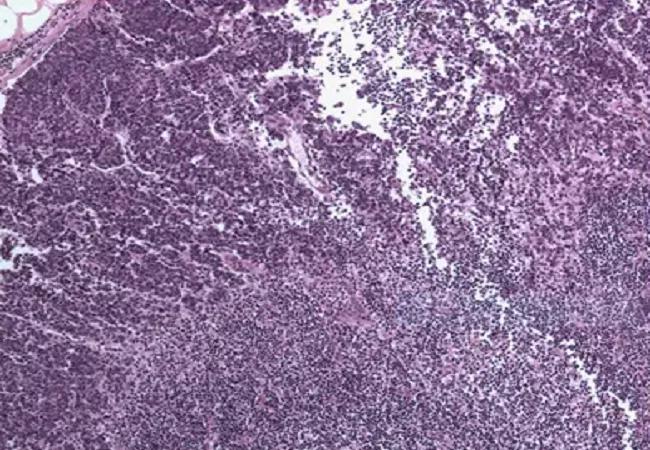
“Merkel cell carcinoma is one of the most immunogenic tumors,” says Dr. Ko. “The tumor cells are small and they can be hard to detect in a whole sea of immune cells that populate the lymph nodes. We wanted to know how patient prognosis was impacted by findings of different patterns of tumor cells seen with immunohistochemical staining, and various amounts of disease on sentinel lymph node biopsy. The impact on prognosis had not been reported in the literature before.”
Advertisement
The team’s analyses provide novel information for management of patients with MCC in three areas:
The team’s initial study was a retrospective review of histologic pattern of SNL in 64 patients with stage III MCC, intended to identify clinicopathologic predictors of outcome. Five metastatic patterns were characterized: a diffuse, sheet-like solid growth of lymph node parenchyma (n-38, 59%); nonsolid, parafollicular growth (n=4, 6%); scattered, dyshesive tumor cells of varying number in the subcapsular sinus, the draining sinuses, or both sites (n=11, 17%); tight perivascular hilar (n=1, 2%); and rare, scattered parenchymal cells (n=1, 16%).
At the time of follow-up, 30 patients (48%) had died and 21 of the deaths (33%) were attributable to MCC. Survival was poorer overall in patients with the sheet-like pattern of metastases than in those with the other metastasis pattern types (p = 0.03), with 22 of the deaths (73%) occurring in patients with the solid, sheet-like pattern. In contrast, three deaths (10%, all involving immunosuppressed patients) were associated with the rare scattered parenchymal cell pattern; four deaths (13%) were associated with the sinusoidal pattern; and one death (3%) was in a patient with the nonsolid parafollicular pattern.
Advertisement
In multivariable analysis, the number of positive SLN (1 or 2 vs. > 2, p < .0001), patient age (< 70 vs. ≥ 70, p = .01), SLN metastasis pattern (sheet-like vs. the other four types, p = .02), and immune status (immunocompetent vs suppressed, p = .03) were independent predictors of outcome. The researchers also found that those characteristics could be used to stratify Stage III patients into three groups with significantly different outcomes.
“This was the first study to investigate the meaning of various patterns of sentinel lymph node involvement by Merkel cell carcinoma, including the meaning of disease identified with immunohistochemistry alone,” says Dr. Ko, the paper’s first author. “Our findings suggest improved survival in patients with metastatic tumor involving sentinel lymph nodes detected only by immunohistochemistry, and raise the question of whether these patients deserve separate classification and different management, analogous to what is standard of care in breast carcinoma.”
The Cleveland Clinic team next took on the challenge of determining what characteristics of MCC are associated with a positive SLN and decreased overall survival (OS). To do so, they analyzed data from 3,048 patients with MCC in the National Cancer Database from 2012 to 2014, of whom 1,174 had undergone SLN biopsy. Predictors of SLN positivity were evaluated using logistic regression. OS was evaluated using a Cox proportional hazards model.
“In our other two studies, we used patient subsets from Cleveland Clinic and cooperating institutions,” says Dr. Ko. “For this analysis, we were fortunate to have access to a huge dataset of patients from across the country. The question we wanted to answer was whether there is a way to narrow down which patients might not need sentinel lymph node biopsy, based on different tumor parameters.”
Advertisement
Multivariate analysis showed that a positive SLN was more likely in patients with MCC who had primary lesions on the trunk (odds ratio [OR], 1.98; 95% confidence interval [CI], 1.23-3.17; p = .004), tumor-infiltrating lymphocytes (OR, 1.58; 95% CI, 1.01-2.45; p = .04), or lymphovascular invasion (OR, 3.5; 95% CI, 2.51-4.76; p < .001). OS was lower in patients who were ages 75 or older (hazard ratio [HR], 2.55; 95% CI, 1.36-4.77; p = .003), male (HR, 1.78; 95% CI, 1.09-2.19, p = .022), immunosuppressed (HR, 3.51; 95% CI, 1.72-7.13; p = .001), and who had a positive SLN (HR, 3.15; 95% CI, 1.98-5.04; p < .001).
At this point, SLN biopsy is still recommended for all MCC patients, Dr. Ko says.
The team’s most recently published research involved the prognostic significance of nonsolid microscopic metastasis in SLN for MCC. The findings suggest that outcomes for patients with nonsolid metastases are similar to those of patients with negative SLN biopsies. The exception is patients with a sinusoidal SLN biopsy pattern, which in the study was associated with worse outcomes.
The researchers retrospectively analyzed the presence and patterns of metastases in 38 patients with MCC: 16 whose SLN biopsies were positive and 22 whose SLN biopsies were negative. Five-level, step-wise sectioning at 250-µm intervals was performed in all SLN blocks, with an immunohistochemical stain for cytokeratin 20 performed on all levels. Median follow-up was 56.3 months overall, and 50.4 months and 66.8 months for the SLN biopsy-positive and biopsy-negative groups, respectively.
Advertisement
OS and disease-specific survival (DSS) did not differ between the two diagnostic groups but did differ by immune status (immunocompetent vs. immunosuppressed, OS p = 0.03), DSS p = 0.005) and primary tumor category (OR p < 0.0001, DSS p = 0.001). On deeper sectioning, all 16 diagnostically positive SLN biopsies continued to show nonsolid microscopic metastasis, and 32% (7/22) of diagnostically negative SLN biopsies revealed nonsolid metastasis. Sinusoidal metastasis was associated with worse DSS than were all other patterns (p = 0.02).
“In this study, patients with the rare-cell pattern — up to 10 cells in scanning magnification — seemed to do just as well as patients who had a negative sentinel lymph node biopsy,” says Dr. Ko. “These data may help us stratify patients with stage III Merkel cell carcinoma according to prognosis and make better choices about the kind of treatment and surveillance they might need.”
Collectively, the Cleveland Clinic team’s findings strongly indicate that nonsolid microscopic tumor cell growth patterns in MCC SLN biopsies represent less aggressive disease than do solid metastatic patterns.
The researchers’ next steps include a study of primary tumor tissue from a cohort of Cleveland Clinic Cancer Center MCC patients treated with immunotherapy, to attempt to understand why some tumors respond to the treatment and some do not.
They also hope that pathologists in other institutions will start including information about MCC cell patterns of SLN involvement in pathology reports. Those data could form the basis of a larger national cohort for studies to validate the findings of the three existing reports.
For clinicians treating MCC patients, the key take-home message from the Cleveland Clinic Cancer Center studies is to look at the whole picture, not just whether a lymph node is positive or negative, according to Dr. Ko.
“Clinicians should consider a patient’s immune status, how many lymph nodes are involved, what the cell pattern is, and whether the pattern was solid or nonsolid,” she says. “Putting all those pieces together will give you a more accurate idea of how well a patient is likely to do and how aggressive treatment should be.”
Feature image: Pattern of lymph node involvement in Merkel cell carcinoma characterized by a solid, sheet-like proliferation of metastatic tumor.
Credit: Ko JS, Prieto VG, Elson PJ, et al. Histological pattern of Merkel cell carcinoma sentinel lymph node metastasis improves stratification of Stage III patients. Mod Pathol. 2016 Feb;29(2):122-30.
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors