New techniques target nerves with improved accuracy, less pain
When it comes to managing hip and knee pain, surgery is not always the answer. Conditions such as morbid obesity, diabetes and severe heart disease may make patients less than ideal candidates for joint replacement surgery. Patients in their 40s or 50s may be considered too young for a joint replacement, since joint replacements only last a limited amount of time. In addition, some patients may continue to suffer from joint pain even after having a hip or knee replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Experts from Cleveland Clinic’s Department of Pain Management offer radiofrequency ablation (RFA) as a minimally invasive method of hip and knee pain management. “For many patients considering a joint replacement, pain is their main motivation for treatment rather than join instability,” explains pain management specialist Jianguo Cheng, MD, PhD. “With RFA, we can still reduce pain and improve functionality, but without the increased risk of complications associated with surgery.”
RFA is a neurolytic technique that uses heat to produce controlled tissue destruction through a process called thermocoagulation. With a radiofrequency of 350,000 to 500,000 Hz, the hot needle tip coagulates the nerve proteins, stopping them from functioning. This targeted nerve destruction interferes with the conduction and transmission of pain signals from the joint to the brain. In patients with hip pain, RFA targets the articular branches of the femoral and obturator nerves. For patients with knee problems, RFA targets the genicular nerves. Although complications from RFA are very rare, they may include nerve and vessel puncture, bleeding and infection.
While RFA has been used to treat back pain since 1975, the past 10 years have experienced the most significant improvements in radiofrequency instrumentation and nerve targeting techniques. According to Dr. Cheng, “The goal of the physician is to place the needle as close to the targeted nerve as possible, which helps maximize the therapeutic effects while minimizing the ablation of nearby body structures.”
Advertisement
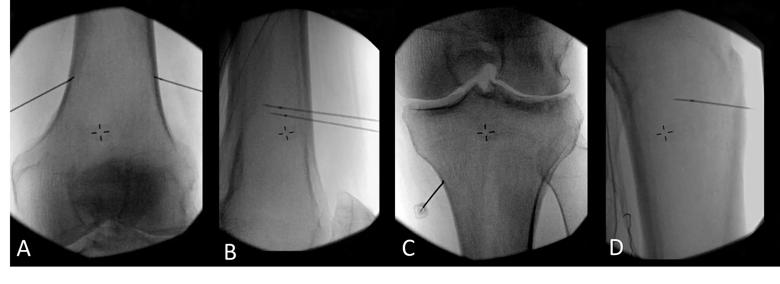
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56005c87-f555-4f43-b5b3-560974f6b0fc/17-PAI-1171-Cheng-Inset-Image-01-650pxl-width-all_jpg)
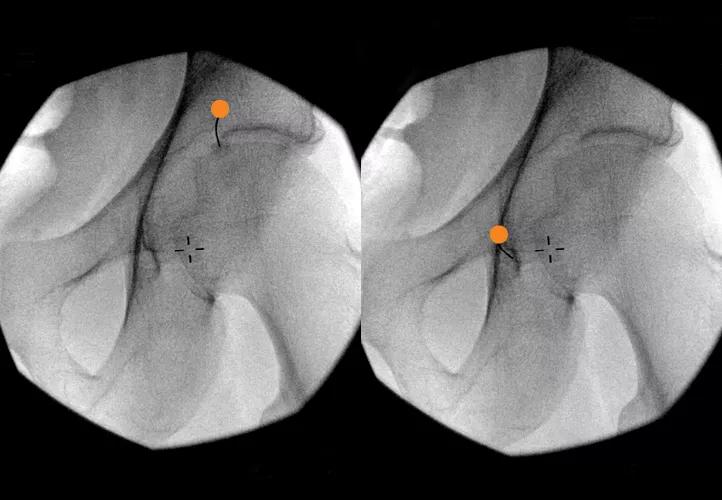
Anteroposterior (A, C) and lateral (B, D) views of probe placement targeting the medial superior genicular nerve (A, B), lateral superior genicular nerve (A, B) and medial inferior genicular nerve (C, D) in the knee joint.
Dr. Cheng’s team recently completed a research project designed to optimize the RFA technique to reduce procedural pain in the knee. “Because the knee is very sensitive to pain and patients are not anesthetized during RFA, it has been reported in literature and observed in our clinic that some patients experience extreme pain during the procedure,” explains Dr. Cheng. “We reduced procedural pain by minimizing the needle penetration distance from the skin to the target nerves and reducing irritation to the periosteum.” This was achieved by collecting magnetic resonance imaging (MRI) data of the knee from various patients and determining the best angle of needle placement.
The hips present some unique challenges related to nerve targeting. Especially in obese patients, excess abdominal fat may make it harder to place the needle in the groin area without puncturing a femoral nerve/artery or penetrating the abdomen. This situation calls for doctors to individualize the path of the RFA needle based on each patient’s body build.
“In these cases, experience really is the best teacher,” says Dr. Cheng. ”The more experience physicians gain in performing RFA in the hip, the more adept they become at targeting the right nerves in patients with a variety of body types.” Even with the help of advanced imaging technology, physicians must gain experience interpreting the images as they strive to find the best path for the needle.
Advertisement
Especially when treating the hip, experienced physicians should perform sensory and motor testing before RFA to get the tip of the needle as close to the target as possible. This stimulation also helps ensure that the needle tip stays away from major motor nerves.
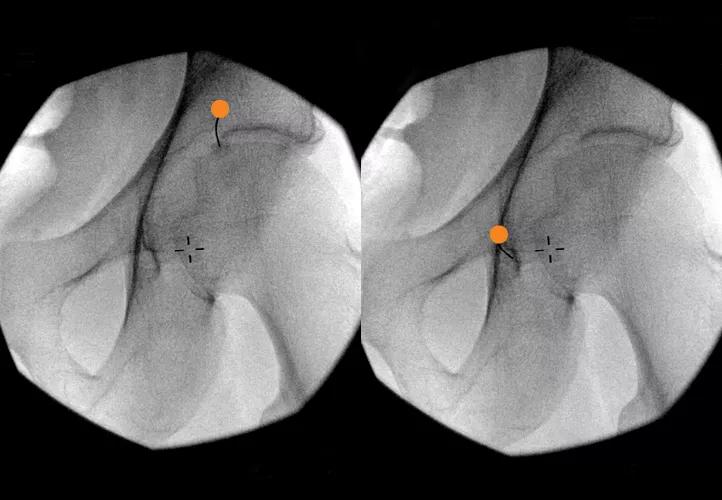
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9b9f2e4f-8f30-4f1c-90a4-9a250b07b5d9/17-PAI-1171-Cheng-Hero-Image-650x450pxl_jpg)
Needle placement targeting the articular branch of the femoral nerve (A) and the articular branch of the obturator nerve (B) in the hip joint. Dots are targets for local anesthetic injection.
RFA works best in patients with isolated joint pain without multiple pain complaints. This pain could be caused by a variety of environmental and genetic factors that have strained their joints. “Patients with severe fibromyalgia or other causes of all-over body pain are not good candidates for RFA,” explains Dr. Cheng. “Unfortunately, treating the hip or knee isn’t going to impact their problems with other connective tissues, which may continue to cause chronic pain.”
Like most medical treatments, individual responses to RFA treatment will vary. Patients with isolated knee or hip pain have reported satisfactory pain relief for three months to two years. Over time, the joint pain is likely to return once the lesioned nerves regrow. However, RFA has been shown to be safe to administer repeatedly in patients with consistent pain reduction results.
Why might pain relief last longer for some patients? According to Dr. Cheng, “there may be different rates of regrowth and regeneration in the nerves. Even with advanced imaging technology, the small size of these nerves makes it very difficult to study and measure the growth rates of nerves.”
Advertisement
“Because we recognize that joint pain can be treated in so many different ways, we are very proactive in developing the best treatment plans for our patients,” comments Dr. Cheng. “In addition to RFA, we augment this technique with a variety of other treatment modalities, including physical therapy, behavioral modification and medications, to maximize comfort and minimize pain.”
Advertisement
Advertisement

Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies

Study participants also reported better sleep quality and reduced use of pain medications

Two-hour training helps patients expand skills that return a sense of control

Program enhances cooperation between traditional and non-pharmacologic care

National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS

Pain specialists can play a role in identifying surgical candidates

Individual needs should be matched to technological features

New technologies and tools offer hope for fuller understanding