Retrospective study involves 18 years of follow-up and shows low risk of local recurrence.

Although some patients with ductal carcinoma in situ (DCIS) choose to undergo lumpectomy and radiation, mastectomy is often recommended in cases of extensive disease, history of prior breast radiation or location that would make achieving negative margins challenging. One open question researchers have sought to understand is the impact on a positive or close (<2 mm) surgical margin on the risk of local recurrence. Researchers at Cleveland Clinic Cancer Center undertook a retrospective study aimed at answering this question.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
After evaluating patient demographics, tumor biology, margin status and therapeutic history for 282 patients with DCIS treated at the clinic between 2000-2010, the researchers concluded that the risk of recurrence after mastectomy for DCIS is low. The data, which was published in the American Journal of Surgery, indicates that recurrence risk is not connected to either margin status or the use of radiation therapy.
In order to decrease the risk that cancer grows back in the area that was surgically removed, it is necessary to achieve a healthy rim of tissue around the cancer, known as a margin. The difficult situation for breast cancer, is that it is microscopic, so the surgeon cannot see the cancer during surgery and must rely on the preoperative imaging to plan the surgery. One the of the risks of surgery is having a positive margin, meaning the cancer is at the margin edge where the surgeon cut to remove it. This “positive margin” potentially could leave some cancer cells remaining in the surgical area, which could contribute to a recurrence.
Studies show that the risk of a local recurrence for patients who undergo a lumpectomy for DCIS is improved with a surgical margin of at least 2 mm width. Whether or not the 2 mm surgical margin is needed for a mastectomy is not known. Historically, if the mastectomy surgical margin was less than 2 mm, patients would be recommended to undergo radiation, to err on the side of caution. However, there is still a debate in the medical community about whether the risks of adding radiation in the setting outweigh the benefits.
Advertisement
For this study, researchers reviewed cases where there was positive or close mastectomy margins for DCIS or microinvasive DCIS (< 1 mm of invasive cancer identified) and then analyzed the management of those cases and tracked instances of recurrence compared to patients with a > 2 mm margin. They then sought to understand whether wider surgical margins and/or adjuvant therapy provided a benefit.
Patient records were analyzed according to four groups:
In total, 12.3% of patients had a positive (9 patients) or close margin (36 patients). The below table summarizes adjuvant therapy received, with 7 patients receiving radiation, 17 receiving endocrine therapy and the majority (216) receiving no further treatment. During the study period, 10 patients (3.4%) experienced a local recurrence. Seven of those patients had a margin of >1 mm, with six having a margin of >2 mm. 89% of patients with a positive margin who received adjuvant radiation and had no recurrence after 12 years.
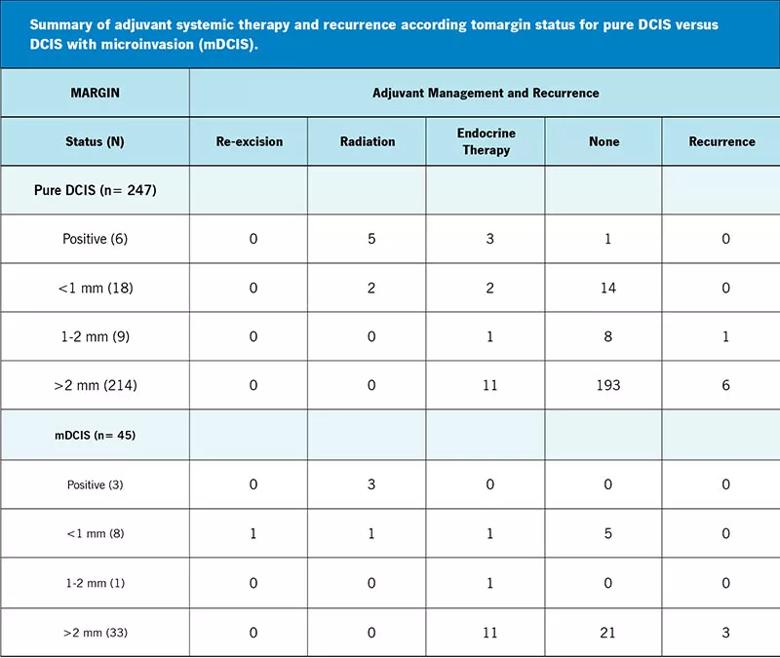
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2b379702-5726-49a0-bce1-9044ad8d2c50/23-CNR-4162208-CQD-Inset-Table-800x675-DCIS_jpg)
“What we found is that among patients who had a positive margin, they all received radiation and none of them recurred. So it’s always possible to consider radiation for these patients,” says Stephanie Valente, DO, Director Western Region Breast and Fairview Hospital Breast Programs and lead author of the study. “However, we also saw that patients who had a positive or close margin who did not receive radiation also did not have a recurrence. Interestingly, patients who had a > 2 mm margin still had a recurrence, so the risk of recurrence did not appear to be related to the margin width.
Advertisement
Even though margins are important, you don’t always want to radiate a margin if the risk of a recurrence is low. The study shows that radiation helps, but it is known that there are serious side effects related to radiation, especially potential damage to the heart or lung, skin as well as risk of secondary cancers like angiosarcoma. Modern radiation equipment and technology have reduced those risks somewhat, but they are still important factors to discuss with patients as part of shared decision-making.
Patients who have a mastectomy no longer need mammograms or MRIs, but should still have a breast exam a few times a year, since if there is local recurrence that most often presents as a lump that can be felt. “The study indicates that it is safe to watch these patients and forgo radiation, because we don’t want to overtreat a population of patients for whom 97% will never have an issue,” says Dr. Valente.
Another common question that comes up is whether patients need treatment to prevent cancer in the other breast after a single mastectomy for DCIS. Another Cleveland Clinic research reported that for some patients, it may be preferable to have a bilateral mastectomy if the alternative is a single mastectomy, followed by five years of taking Tamoxifen to protect the other breast, since the medication has numerous side effects such as early menopause and increased risk of endometrial cancer. “Many patients don’t want to take medication, and especially with the amazing reconstruction that’s out there, we are seeing more women opting for bilateral mastectomy,” says Dr. Valente. Further studies from Cleveland Clinic noted that the complication rate between one-sided and bilateral mastectomy is exactly the same in healthy women.
Advertisement
People often have a perception that surgeons can visually identify cancer tissue during excision so that they can get clear margins, but currently that is not possible. The surgeon must send the tissue to pathology and wait several days to a week to ascertain this information. The research team is now participating in national clinical trials to determine if there are imaging or other modalities that could be performed during surgery to guide surgeons in obtaining clear margins. This would be a crucial step forward in advancing breast cancer care.
Advertisement
Advertisement

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Reconsidering axillary lymph node dissection as well as depth of surgical margins

Ultra-Hypofractionated Whole Breast Irradiation and Partial Breast Irradiation Reduce Many Toxicities

Best practices for reducing toxicities

Partnerships with local social service agencies key to program success

Ongoing clinical validation refine breast cancer risk substratification

Phase 3 trial found no survival differences between weekly or biweekly doxorubicin/cyclophosphamide or between weekly or biweekly paclitaxel

Findings strengthen evidence for risk-reducing procedures