Viewpoints from Steven Wexner, MD, PhD (Hon)
Numerous studies undertaken during the last 15 years have failed to show any advantage conferred by robotics as compared with laparoscopy when performing total mesorectal excision (TME) for rectal cancer. Conversely, most studies have found significantly longer time and significantly greater expense when the robotic technology has been employed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
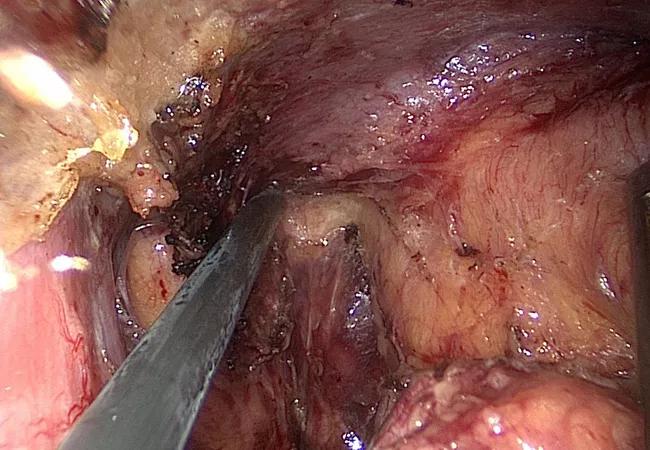
However, it has also been well established that any form of minimally invasive surgery, whether laparoscopic, hand-assisted, single-port or robotic is superior to a laparotomy. One of the most accomplished robotic surgeons in the world, if not the most accomplished, is Seon-Hahn Kim, MD, PhD, from Korea University School of Medicine. Dr. Kim recently published his results of minimally invasive surgery for rectal cancer between April 2007 and March 2014.
He and his group began with 732 patients, 460 of whom underwent laparoscopy TME, while an addition 272 patients underwent robotic resection. They analyzed all of the usual parameters. As has been previously demonstrated by numerous authors, the operative times were significantly longer in the robotic group at 285.8 vs. 249.7 minutes in the laparoscopic group (P < 0.0001). Moreover, the incidence of postoperative ileus was more than double in the robotic group (12.1% vs. 5.4% laparoscopic, P = 0.018). There were some skewing between the groups in that the patients in the robotic group were significantly younger at 59.2 vs. 63.9 years (P < 0.0001) and had fewer morbidities than did patients in the laparoscopic group.
Not surprisingly, the patients in the both of Dr. Kim’s groups were asthenic with mean BMIs of 23.5 kg/m2 in the robotic group and 23.3 kg/m2 in the laparoscopic group. In order to make the groups more equivalent, Dr. Kim and his colleagues matched 224 of the patients who underwent robotic TME with 224 patients who underwent laparoscopic TME. Whether matched or unmatched, the authors failed to identify any significant benefit conferred by robotic surgery relative to overall survival, cancer specific survival or disease-free survival.
Advertisement
One additional factor which should have been in favor of the robotic group is that preoperative chemoradiotherapy had been employed in 31.6 percent of the patients who underwent robotic surgery vs. only 13.5 percent of patients in the laparoscopic group (P < 0.0001). However, again, even with matching, the only differences which the authors were able to identify were an increased operative time and an increased incidence of prolonged postoperative ileus. They did not evaluate cost. It is interesting that despite the fact that the authors were unable to identify any statistically significant benefit to robotic TME, they note that there was “no deterioration of long term survival outcomes” and that the “oncologic advantage” “is partly demonstrated with this study and may be further evidence through future studies.”
I applaud the authors for the size of their series as well as for their honesty in reporting their results. It is somewhat difficult to imagine how if one of the world’s masters of robotic surgery cannot confer any additional advantage over laparoscopy how other less experienced surgeons may be able to do so. Nonetheless, I am sure that we will read many more studies in which surgeons continue to attempt to prove that robotic TME has an advantage compared with laparoscopic TME. Perhaps some day that this postulate may be proven true. For now, we can safely conclude that any minimally invasive procedure ― whether laparoscopic, hand-assisted, single-port or robotic ― is superior to an open operation. These data from Kim and co-workers, like a myriad of prior publications, do not offer any compelling reason for skilled laparoscopic rectal cancer surgeons to embrace the robotic method. However, if the robotic platform can help surgeons migrate from open and perhaps even hand-assisted operations to this more minimally invasive modality, then an important achievement will have been made.
Advertisement
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications