Panel outlines research priorities around a promising alternative to imaging markers
The next stages of research into the potential of serum neurofilament light as a biomarker in progressive multiple sclerosis (MS) should focus on its use to predict disease course and to detect and monitor response to treatment. So concludes a new report from an expert panel convened by the International Progressive MS Alliance and published as an open-access “Views & Reviews” paper in Neurology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A major challenge in the development of therapies for progressive MS has been identification of a biomarker to use in early-stage trials. While neurofilament light is viewed as holding potential utility, it needs further development.
“The lack of a rapid means to determine whether a therapy is working has been an obstacle to development of treatments to stop worsening disability in progressive MS,” says Cleveland Clinic neurologist Robert Fox, MD, a co-leader of the expert panel and corresponding author of the summary paper. “Interest has grown in serum neurofilament light as a potential tissue fluid biomarker to serve this purpose and overcome the limitations of imaging biomarkers, so the Alliance convened our group to assess its potential and identify priorities for further research.”
While lesion activity on MRI has served as a useful means of monitoring patients with relapsing MS, disease activity is less easily measured in progressive MS, as it usually happens more slowly. This has limited the utility of imaging biomarkers in phase 2 proof-of-concept studies of therapies for progressive MS, contributing to the shortage of effective therapies for progressive MS.
“Body fluid biomarkers demonstrate potential to be more pathologically specific than imaging markers, which suggests they may reflect pathology throughout the entire central nervous system and thus may better indicate the effects of systemic treatment,” explains Dr. Fox, staff in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research.
Advertisement
For this reason, the International Progressive MS Alliance — whose mission is to accelerate development of therapies for progressive MS — increased its attention on body fluid biomarkers. The group decided in mid-2018 to focus on one of them — neurofilament light chain (NfL) — as a test candidate, for two main reasons:
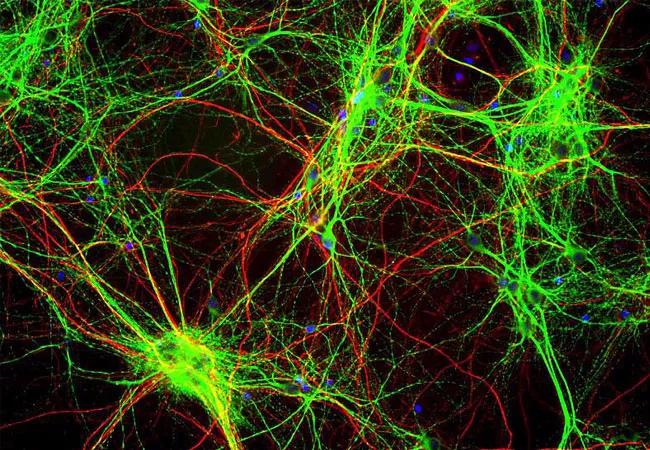
Neurofilaments are proteins that serve to maintain the nerve cell structure required to enable proper electrical impulse conduction via axons. NfL in particular is part of the debris that enters the CSF and blood following damage to axons due to MS or other causes.
Studies of NfL in serum and plasma have been undertaken to determine how best to use this marker to detect and predict disease progression and treatment response in MS and other neurologic diseases. Recent clinical trials have used periodic NfL monitoring to assess effects in both relapsing and progressive MS.
As detailed in their paper in Neurology, the expert panel concludes that serum NfL “is a plausible marker of neurodegeneration that can be measured accurately, sensitively, and reproducibly.” They note that data from cohorts with relapsing and progressive MS are similar and show that serum NfL levels correlate with imaging and disability measures, serve to predict future disease activity and can predict response to treatment.
Advertisement
“Evidence suggests that disease activity from active inflammation — as indicated by new T2 and gadolinium-enhancing lesions on imaging — is an important contributor to serum NfL levels, so it won’t be easy to distinguish this disease activity from the disease progression that fuels the insidious disability progression observed in progressive MS,” says Dr. Fox.
The panel identified two “contexts of use” for further investigation of serum NfL in progressive MS:
The panel also called attention to three things needed before NfL can be accepted as a biomarker in progressive MS:
The panel’s full “Views & Reviews” paper is available here.
Image at top courtesy of Wikimedia Commons under the Creative Commons Attribution license
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help