Calcium is an integral component of atherosclerotic plaques, and the extent of coronary calcification correlates with success rates, complication rates, acute luminal gain and subsequent restenosis rates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
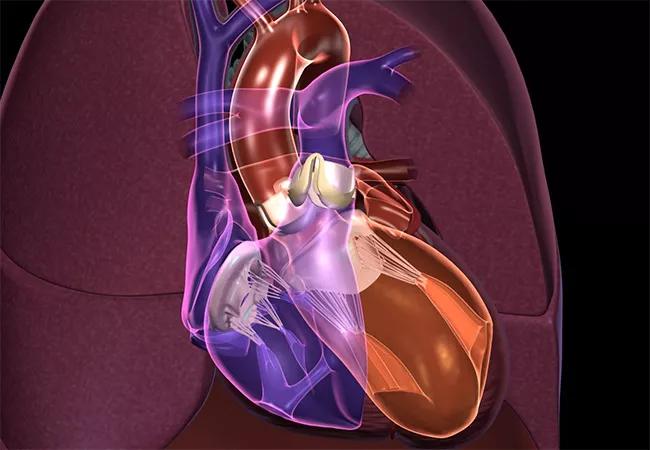
The pattern of plaque calcification directly affects the complexity, risk and outcome of percutaneous procedures in both the coronary and peripheral interventions. The deposition of calcium in plaque is not uniform. In the vessel wall, it may be eccentric or circumferential, luminal or deep in the wall, relatively focal or quite diffuse. The calcification pattern directly affects the radial compliance, vessel flexibility and luminal resistance to the passage of interventional equipment.
Several devices and strategies have been developed to address coronary calcification, including rotational atherectomy, cutting and sculpting balloons and off-label use of laser-contrast detonation. These devices are sufficient to treat many patterns of coronary calcification but are limited in their efficacy at treating deep circumferential calcium.
It is not uncommon to encounter “non-dilatable” lesions that fail to expand within rated balloon burst pressures despite atherectomy. Over-pressurizing or oversizing balloons, aggressive repeat atherectomy or off-label laser contrast detonation may be successful but carry substantial risk of perforation, rupture, dissection or abrupt vessel closure. The alternative strategy of deploying a stent within the under-expanded segment is a frequent cause of in-stent restenosis and target lesion failure.
Shockwave intravascular lithotripsy (IVL) was recently approved in the United States for use in the coronary circulation. IVL has been used in the peripheral circulation in the United States for several years, with FDA approval of the peripheral lithotripsy device in 2016. Coronary interventions have been available and approved in Europe since 2018.
Advertisement
IVL is indicated for de novo treatment of severely calcified lesions in the coronary arteries. It is complementary to current atheroablative technologies such as orbital (CSI Technologies) and rotational (Rotablator™, Boston Scientific) atherectomy.
These rotational ablative technologies are irreplaceable for treating long, diffusely calcified lesions with mixed superficial and deep calcium. They play a crucial role in napkin ring lesions where other devices fail to cross.
Compared to vessel preparation with balloon angioplasty, however, rotational/orbital atherectomy devices have several limitations. Foremost is a steep learning curve to proficiency and comfort in the use of atherectomy. The devices are cumbersome to set up and require the operator and assisting technologist to be facile with long wire exchanges.
Catastrophic complications such as coronary perforation or no reflow are more common than with balloon angioplasty. And there are unique complications such as burr stall, burr entrapment and wire transection that can suddenly occur with catastrophic consequences. Concern for these factors can foster a bias towards underutilization of atheroablative techniques commonly referred to as “rotablator regret.”
IVL is attractive for its ease of use and safety profile. It preps like a standard balloon and delivers like a stent. The coronary balloons are 12 mm in length and charged to deliver eight 10-second treatments. The IVL balloons are inflated to four atmospheres with a standard saline contrast mixture. Each coronary balloon has two emitters that are electrified and cause instantaneous vaporization of a saline contrast solution. This results in the rapid expansion and collapse of a bubble, sending sonic pressure waves through the tissue with an effective pressure of 50 atmospheres.
Advertisement
Each lesion treated requires at least one — and often all — the charges in the balloon. Shockwave lithotripsy balloons are, therefore, most effective at fracturing superficial and deep calcified lesions in limited length segments. IVL alters vessel compliance, allowing dilation of lesions at low pressure.
IVL is not approved for use within stents because of concerns for damage to the polymer coat and alteration in drug delivery of current drug-eluting stents. This new technology is more expensive than atheroablative technologies or traditional balloons but is reimbursed as of July for outpatient procedures and will be for inpatient in November via a new technology add-on payment (NTAP).
IVL is clearly a breakthrough technology allowing interventional cardiologists to successfully treat, with a very safe and easy-to-use technology, coronary lesions that were previously untreatable. Since the device became available in our lab, we have found it to be an extremely useful addition to our armamentarium – within the first two weeks of having it we used it in about a dozen cases.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.