Preop rad therapy can offer reduced treatment duration, improved long-term functioning
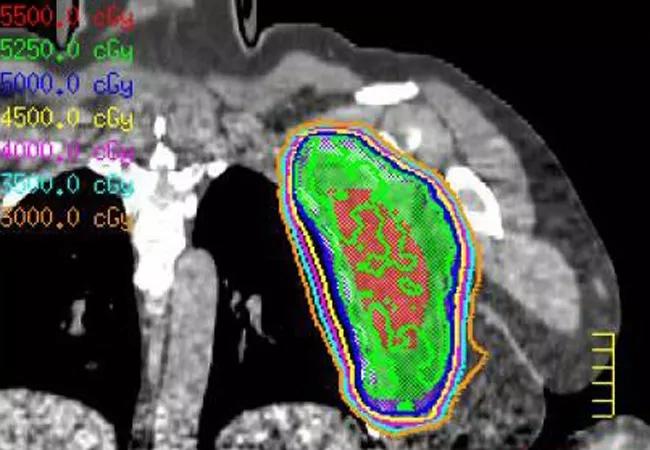
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/75b827af-92a7-4b9b-be70-b94a00dc7344/Sarcoma-treatment_650x450_jpg)
Sarcoma-treatment_650x450
Here’s a suggestion for physicians confronted with a case of soft-tissue sarcoma or suspicious mass: consider advising your patients to delay surgery until they are evaluated by an orthopedic oncologist, medical oncologist, musculoskeletal radiologist and radiation oncologist, preferably with sarcoma experience. They will form a multidisciplinary team to evaluate and optimize a treatment plan for the patient, including the biopsy approach with evaluation by a pathologist specialized in sarcomas.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Why? Because some of the masses may be soft-tissue sarcomas, and sarcomas, particularly intermediate- and high-grade sarcomas, can be treated with preoperative radiation therapy followed by surgery, rather than surgery followed by postoperative radiation therapy. According to clinical trial data, this approach can improve long-term quality of life and overall functioning.
“Patients often, in a very instinctual way, have the reaction of, ‘I have a mass, I want it taken out right away,’” says Chirag Shah, MD, a radiation oncologist at Cleveland Clinic Cancer Center and co-author of two recent consensus papers on treatment of soft-tissue sarcoma. “You often have to fight that gut instinct.”
Soft-tissue sarcomas represent a rare and complex constellation of malignancies originating throughout the body. Approximately 12,000 new cases are diagnosed every year in the United States, and first-line treatment approaches range from amputation to limb preserving surgery with or without radiation therapy.
Preoperative radiation has not demonstrated an improvement in survival compared to postoperative radiation but instead shortens the duration of radiation therapy and offers the potential for improved long-term functioning by reducing fibrosis and joint stiffness, according to Dr. Shah.
Five-year survival rates remain consistent between postoperative and preoperative radiation therapy for soft-tissue sarcomas, according to a 2016 review from Dr. Shah and the sarcoma treatment team at Cleveland Clinic. However, there are still many good reasons to think radiation first, he says.
Advertisement
Potential benefits of preoperative radiation, as compared to a postoperative approach, include shorter duration of treatment, lower total radiation dose, smaller area requiring radiation, reduction in long-term side effects, and improved overall long-term functioning.
Potential disadvantages include higher potential for postsurgical wound complications and the possibility of disease progression during the course of radiation.
“Soft-tissue sarcoma can be unfamiliar not only to patients but also to many physicians, who may practice their entire careers and never encounter a single case,” says Dr. Shah. “Development of ideal treatment plans, therefore, can be challenging for providers and surgeons.”
Particularly in intermediate- and high-grade sarcomas, radiation therapy can, and often should, be considered before surgery.
A randomized trial in the 1970s and 1980s confirmed equivalent survival rates between amputation and limb-sparing surgery followed by postoperative radiation. However, more than 30 years since publication of these early studies, nearly one-third of patients with soft-tissue sarcomas fail to receive even postoperative radiation therapy following limb-sparing surgery.
Dr. Shah considers that to be the result of poor understanding among practitioners and surgeons about the benefits of radiation in the treatment of soft-tissue sarcomas. It’s also a good reason why physicians should consult with sarcoma experts, including surgeons and oncologists early in treatment planning, he says.
Advertisement
“By bringing sarcoma specialists into the planning process, you create a collaborative environment where each patient is treated as an individual and the treatment team can recommend customized approaches that draw on the expertise of everyone involved,” says Dr. Shah.
“Benefits of this include reduction in the number of overall procedures, reduced complications, and improvements in overall quality of life and long-term functioning.”
As with any type of cancer, details matter when planning treatment for soft-tissue sarcomas.
“Not every patient needs radiation, but getting the opinion of a radiation oncologist familiar with sarcomas makes sure that they are evaluated for the optimal treatment, rather than treated in a one-size-fits-all approach,” says Dr. Shah
For example, sarcoma patients with a higher risk of local recurrence are more likely to realize maximum benefits of radiation therapy.
Indications for higher likelihood of local recurrence and therefore potential benefit to radiation therapy include tumor size larger than 5 cm, deep tumor site, high grade, recurrent disease, or closely resected margins.
“All of this emphasizes the importance of bringing a dedicated team into the treatment planning process as early as possible,” says Dr. Shah. “We can help clarify when radiation represents the best option for patients and when up front surgery may be the better choice.”
Dr. Shah is associate staff in and Director of Clinical Research for the Department of Radiation Oncology at Cleveland Clinic Cancer Center.
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality