Cardiac dosing 50 percent below national average
When Chirag Shah, MD, became a radiation oncologist in 2007, almost all breast cancer patients had one option: five to six weeks of daily, whole-breast/chest-wall radiation, regardless of surgical type (mastectomy or lumpectomy). A mere decade later, thanks to advances in the field in part refined at Cleveland Clinic Cancer Center, patients can choose among several options for radiotherapy, many of which are far safer for the heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cardiac toxicity after radiotherapy can include a range of conditions, from valvular disease to coronary artery disease and arrhythmias. Accelerated partial-breast irradiation (APBI) is a cardiac and pulmonary dose-sparing technique that allows appropriately selected patients with early-stage breast cancer to complete adjuvant radiation in two weeks or less following breast conserving surgery. To date, multiple randomized trials have demonstrated no difference in rates of recurrence or survival with APBI delivered using brachytherapy or external beam radiation techniques.
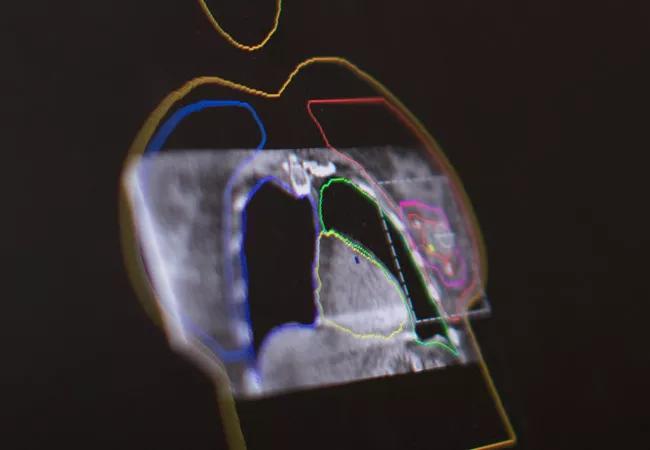
One method of delivering APBI is intensity-modulated radiation therapy (IMRT), a highly precise form of radiotherapy. IMRT is commonly used to treat prostate, head and neck and central nervous system cancers. Dr. Shah’s team is refining its use in breast cancer to deliver partial breast irradiation. IMRT can deliver higher doses with fewer side effects and reduced treatment toxicity, but it does require more planning than other traditional methods.
While techniques targeting a smaller volume area like APBI and intraoperative radiotherapy (IORT) are important for reducing cardiac exposure to radiation, Cleveland Clinic Cancer Center also employs a variety of additional techniques to further minimize cardiac toxicity after radiotherapy for patients requiring more comprehensive radiation therapy to the whole breast/chest wall.
Deep inspiratory breath hold (DIBH)
“The timing of radiotherapy with respect to the breathing cycle can make a clinically significant difference in the dose the heart receives,” says Dr. Shah. “We incorporate this timing into our treatment planning by having patients perform a deep inspiratory breath hold during the CT scan used for planning, and we can estimate doses to the heart and observe the benefit with DIBH as compared to without.” For daily treatment, the active breathing control (ABC) system tracks the patient’s breathing, using the amount of air inspired as a surrogate for the distance between the heart and the breast. At the designated distance (based on inspiratory volume), the radiation is delivered. Surface-guided radiation therapy is used to ensure that the technique is delivered with accuracy.
Advertisement
Prone technique
Prone patient positioning allows the breast to fall away from the chest wall, increasing the distance of the radiation beam from the heart and reducing cardiac dose. “It’s especially useful for patients with large breasts,” says Dr. Shah. “It doesn’t make as big of an impact as using breathing techniques such as DIBH, but it can be beneficial for a subset of patients.”
Heart blocks
Heart blocks represent another strategy to reduce cardiac dose. During treatment planning, Dr. Shah and the team block the heart using computer-programmed leaves inside the linear accelerator. The advances in programming allow blockage of the left ventricle without sacrificing dosing to the breast/chest wall. Using blocks allows for further reduction in heart dose and can be used with DIBH and other techniques.
The team is preparing data for publication showing that cardiac doses at Cleveland Clinic are lower than the national standard by more than 50 percent. “If you exclude the most complicated cases treating targets near the heart, the average is closer to a 75 percent reduction,” says Dr. Shah. “We’re really proud of what we’ve been able to achieve for our patients using a combination of cardiac-sparing techniques.”
The next step, says Dr. Shah, is working with colleagues in medical oncology and cardiac oncology to study the impact of breast cancer treatment on the heart in a multidisciplinary manner. “We’re looking at the impact of treatment factors such as radiation and chemotherapy, as well as non-treatment factors such as high blood pressure, high cholesterol, really a variety of factors to identify a way to risk stratify breast cancer patients and survivors to determine the optimal treatment and cardiac follow-up regimens for each patient,” says Dr. Shah.
Advertisement
With a variety of innovations and radiation technique trials available to patients, Dr. Shah is optimistic about the ability of breast radiation oncology to increase its impact on patient survival and quality of life. “In the short years I’ve been practicing, the field has exploded with better options for patients, and I believe we’ve only just begun.”
Photo Credit: Russel Lee
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists